Relationship between maxillary disjunction and level of asthma control in school-aged patients
Sáenz-Guerrero, Gilberto1; Pacheco-Santiesteban, Rosaura1; Soto-Ramos, Mario2; Monreal-Romero, Humberto Alejandro1; Martínez-Mata, Guillermo1
Sáenz-Guerrero, Gilberto1; Pacheco-Santiesteban, Rosaura1; Soto-Ramos, Mario2; Monreal-Romero, Humberto Alejandro1; Martínez-Mata, Guillermo1
ABSTRACT
KEYWORDS
Asthma, rhinitis, maxillary disjunction.Introduction
In order to understand the close relationship between respiratory function and the development of the stomatognathic apparatus, we must remember that the function is closely related to growth and development, in such a way that through nasal breathing multiple nerve endings are stimulated that generate diverse responses such as the amplitude of thoracic movement, three-dimensional development of the nostrils, ventilation and the size of the maxillary sinuses, but which also induce the growth and remodeling of the adjacent orofacial structures, as well as the transverse development of the maxilla and the direction of facial growth.1 Some researchers claim that nasal obstruction is associated with chronic mouth breathing, constituting the main etiological factor of anomalous craniofacial development, manifesting clinically as vertical facial growth or long face syndrome with subsequent dentomaxillary deformities.2 Among the main stomatological manifestations, deep and narrow palates characterized by inverted V-shaped arches and an increase in palatal depth are reported, with a consequent maxillary protrusion, developing in most cases a class II subdivision 2 malocclusion, also known as distal dysgnathia, associated with mandibular retrusion.3,4 In addition, mechanical obstructions of congenital origin have been found, such as choanal atresia, alterations in Waldeyer's ring and other endonasal obstructions, as well as physiological alterations of the airways, which if not resolved in time may cause dentocraniofacial deformities.4 The prevalence of asthmatic problems has been increasing during the last years, rising from 3.2 to 25%, being considered the most frequent chronic respiratory disease.5 In Mexico, asthma affects from 5 to 8% of the population, with variations among the different regions of the country.6 The prevalence of asthmatic problems has been on the rise in recent years, increasing from 3.2 to 25%, being considered the most frequent chronic respiratory disease.5 In Mexico, asthma affects 5 to 8% of the population, with variations among the different regions of the country.6 Thus, the states of Colima, Tabasco, Chihuahua, Yucatán and Mexico City are those with the highest incidence figures of bronchial asthma.7,8 Multiple epidemiological, pathophysiological and therapeutic studies have demonstrated the association between allergic rhinitis and asthma; 90% of patients diagnosed with asthma have allergic rhinitis,9 making it the most frequent chronic disease10 and the most common childhood allergic disease.11 It is clinically defined as a symptomatic disorder of the nose induced by immunoglobulin E (IgE)-mediated inflammation of the membranes lining the nose following exposure to an allergen.10 Asthma and allergic rhinitis are chronic respiratory diseases that obstruct the upper airways,12 inducing an alternative mode of breathing and contributing to breathing through the mouth,7-9 resulting in orofacial developmental disorders, with dental malocclusion being the most frequent manifestation and of greatest interest to the pediatric stomatologist.13 The development of the craniofacial mass and specifically the components of the stomatognathic apparatus may be altered in the presence of a nasorespiratory obstruction, since if nasal breathing is compromised, it is compensated by oral breathing,14 which causes an imbalance between the lips, buccinator muscles and tongue, exerting an abnormal force on the vestibular and lingual faces of the teeth, resulting in dental malpositions, mainly in the transversal direction.15
However, the severity of asthma can change over time and depends not only on the severity of the underlying disease but also on its response to treatment.16 Asthma and allergic rhinitis have been defined as chronic inflammatory airway diseases, which are closely related, especially in childhood, and are manifested by both upper and lower airway obstruction, emphasizing that for good asthma control it is important to adequately control allergic rhinitis, as lack of control of the latter leads to a suboptimal level of asthma control.17 In the most recent revision of the global initiative for the treatment of asthma GINA 2021, it is established that asthma should be evaluated periodically to verify the level of control of the disease and it is classified as: completely controlled, partially controlled or not controlled at all, as well as to perform pulmonary function measurements by means of spirometry or flowmetry, which allows determining the risk of possible later complications. Likewise, in cases where good control is not achieved, it is recommended to investigate adherence to treatment and the correct technique for the use of inhaled medications, as well as adverse environmental factors, comorbidities such as allergic rhinitis, rhinosinusitis, obesity, among others.
The objective of this research work was to establish how pediatric patients with a diagnosis of asthma and with strict pharmacological control of asthma, who present long face syndrome due to being chronic mouth breathers, can improve their pulmonary function by receiving a dentofacial orthopedic treatment, specifically, rapid maxillary expansion.
Material and methods
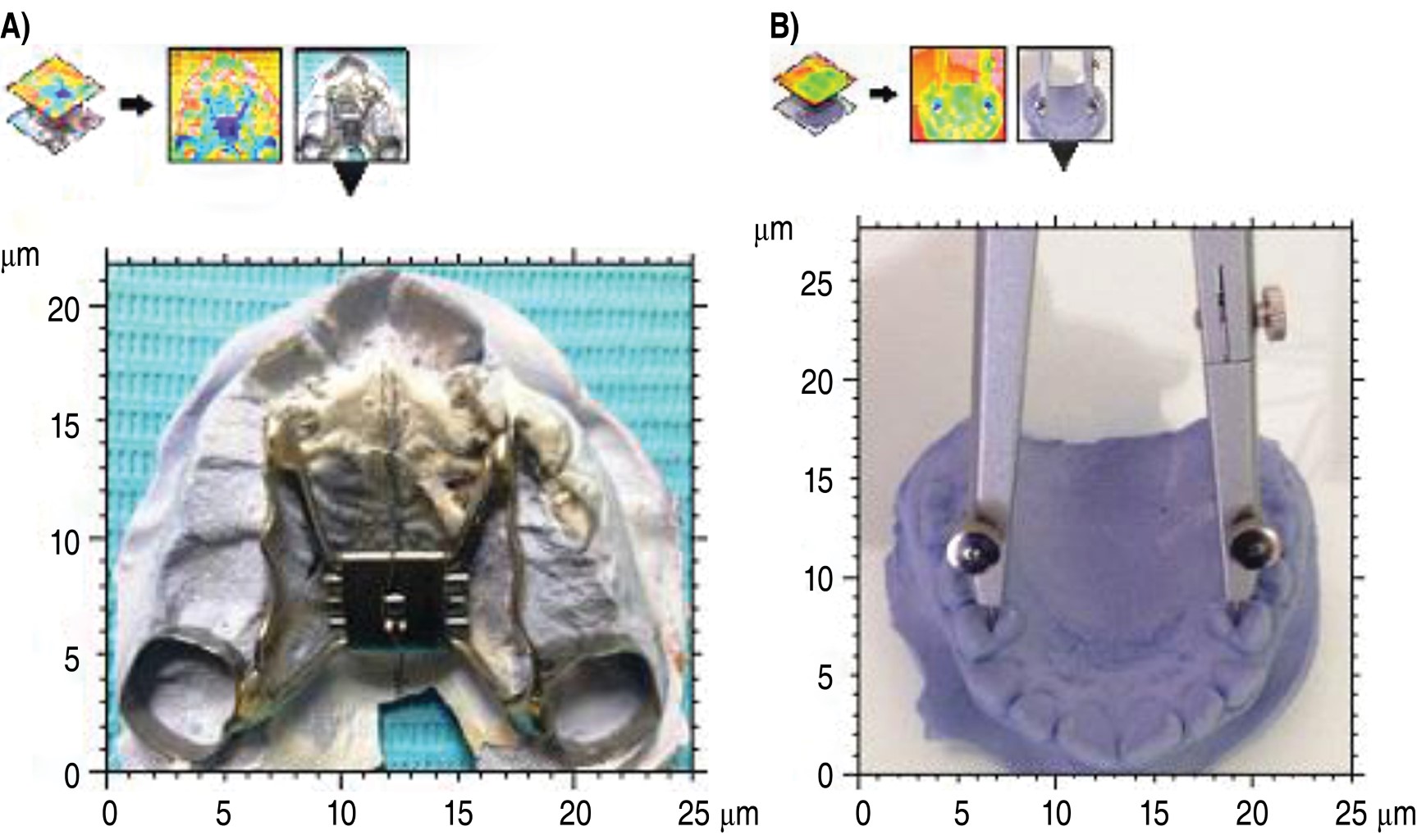
The sample consisted of 15 patients who attended the Pediatric Pneumology Service of the Hospital Infantil de Especialidades del Estado de Chihuahua, aged between 7 and 12 years, all of whom had a baseline diagnosis of asthma and allergic rhinitis. These patients were under strict pharmacological control; However, when they were checked by the pediatric stomatologist, long face syndrome and maxillary compression in a transversal sense were observed, which we consider to be a factor that can interfere in the maximum results that can be obtained with the pharmacological medical treatment, for which reason, with previous authorization of the parents, each one of them was given a stomatological file that included diagnostic aids such as panoramic X-rays and study models, as part of the treatment and follow-up by the Pneumology Service, the patients were evaluated on four occasions, with a time interval of 30 days between one evaluation and another. The first intervention consisted in the evaluation of asthma control by the treating pulmonologist, applying the Asthma Control Test (ACT), with the presence of the pediatric stomatologist to determine if despite being well controlled the patient presented long face syndrome and transverse compression of the maxilla.
The following protocol was followed during the four visits: first the ACT test was performed, then spirometry was performed with an EasyOne® ultrasonic spirometer to determine the values of forced vital capacity (FVC), forced expiratory volume in the first second (FEV1), as well as the FEV1/FVC ratio, and finally a bronchodilator was applied, and after 20 minutes the spirometry was repeated in a comparative manner.
Results
ACT test. Of the patients who attended the pulmonology office of the Hospital Infantil de Especialidades de Chihuahua, 15 participated in this research protocol, who were under strict pharmacological control, with a minimum treatment time of six months, such treatment was focused on the control of asthma and allergic rhinitis, the sample consisted of 10 male patients and five female patients, between the age ranges of seven to 12 years, with a mean of 8.46 and a SD of 1.50 years. The age at which patients were diagnosed as asthmatic ranged from five to 96 months, with a mean age at diagnosis of 39.53 months (3.2 years) and a SD of 24.60 months (2.05 years). All patients underwent a space analysis, obtaining the degree of transverse maxillary compression, where a mean compression in the anterior segment of 4.6 mm was observed, and in the posterior segment of 5.2 mm, with a SD of 1.5 and 2.4 mm, respectively. It is important to mention that when there is a transverse compression of the maxilla, the palate becomes deeper at the expense of the floor of the nostrils. An anterior maxillary compression standard deviation of 1.5 mm and a posterior maxillary compression standard deviation of 2.4 mm was obtained.
Based on the results obtained in the ACT test, it was observed that all the patients in the sample had good or acceptable control of their clinical condition, since their score was equal to or greater than 20 points as an effect of the continuous pharmacological treatment they had at least six months before entering the study. However, the patients clinically manifested adenoid facies and long face syndrome, a sign that the patient is a mouth breather, which almost always causes maxillary compression, a manifestation corroborated by the pediatric stomatologist at the first visit, as previously mentioned. Spirometry studies were also performed in all visits to each of the cases as part of the objective evaluation of asthma control by measuring pulmonary function according to age, weight and height and thus FEV1 and its predicted percentage, FVC and its predicted percentage and the FEV1/FVC ratio were obtained. It should be noted that spirometry provides an objective measurement to determine airway obstruction in patients with asthma and to measure the level of severity of airway obstruction. The FEV1/FVC ratio allows determining the presence of airway obstruction, since normally this index should be greater than 0.8. When it is less than 0.8, an obstructive pattern is defined in the spirometry and to classify the degree of obstruction the FEV1 result is used compared to its predicted value, leaving this classification of obstruction as described in Table 1.
The FEV1 values obtained were equal to or greater than 85% of the predicted value from the first visit or visit zero (Table 2), indicating good asthma control due to strict adherence to pharmacological treatment; however, it can be observed that at visit three there was a significant increase in the same reaching values of 89.6% of the predicted FEV1, here the variable included was the rapid decompression of the maxilla in a transverse direction. This allows us to suggest that such decompression favors pulmonary function. The above data were verified with a Pearson correlation where we found that the highest correlation was between the percentage predicted at visit two and visit three. There is a statistically significant increase from visit one, increasing and lasting the effect until visit three (Table 3).
As part of the protocol, spirometry with application of a bronchodilator was performed 20 minutes after the baseline spirometry, for comparative purposes, by obtaining the average percentage change using the following formula:
(FEV1 post BD - FEV1 baseline)
Baseline FEV1 = % change
When the percentage change is greater than 12% there is a significant change and thus the volume measured in milliliters was using the following formula: FEV1 post BD - FEV1 basal, when it is more than 150 mL (200 mL), we have a significant change.
The mean percentage change was less than 12%, which indicates that there is no significant change after the application of the bronchodilator, which means that most patients were well controlled pharmacologically, although between visits zero and one some cases showed an increase of more than 12%, which indicates that despite the pharmacological treatment at the time of maxillary expansion, an additional improvement in pulmonary function was obtained, as shown in cases 6 and 14 of Table 4.
A Pearson correlation was made between the percentages of change and maxillary compression and the following was found: there is a statistically significant and positive correlation between anterior and posterior compression (0.77), which means that as the anterior maxillary compression increases, so does the posterior maxillary compression. The percentage of change between visit zero and visit one is also positive (as the percentage of change between visit zero increases in this sample so does that of visit one (0.70), that is, as maxillary expansion increases the percentage of change, this effect was also observed in visit two (0.59) although to a lesser degree and visit three (0.67) (Table 5).
Due to the great demographic variability in the country on the prevalence of asthma and rhinitis in children and adolescents, the results shown in this research are conclusive to represent a statistical behavior with positive bias, since it is more common to find values above the value of zero and not below zero, which would show the total absence of such clinical manifestations.
Discussion
In the present study, the ratio of asthmatic patients corresponds to a ratio of 2:1 with respect to gender, that is, it is more frequent in the male gender in pediatric age. Most orthopedic treatments in asthmatic patients are aimed at increasing nasal airflow by disjunction of the maxilla, decreasing airflow resistance from 45 to 53%.17 When the mid-palatal suture is expanded, nasal airflow capacity is increased when measured at maximal effort.18 Other authors have evaluated the changes in nasal airflow after rapid maxillary expansion, with a significant increase in airflow through the nasal passage.19 It is important to mention that none of the studies found in the literature review performed a measurement like this, being that spirometry is a useful, reliable and accessible tool in tertiary hospitals such as the Hospital Infantil de Especialidades de Chihuahua. It is worth mentioning that the maximum improvement in pulmonary function measured by spirometry was observed three months after maxillary expansion, which had not been previously reported by other authors. In this study it is observed that the implementation of the maxillary expansion treatment significantly improved the level of clinical control of asthma as measured by the ACT questionnaire. To show the involvement of the disjunctor during expansion, we propose the following mechanism: due to the fact that disjuncture allows bone separation and this in turn exerts a tension on the palatal suture, a stimulation of osteoblastic activity is generated for bone formation function through the generation of mechanical stress between the sections of the maxillary bone with the consequent production of mediators such as prostaglandins, nitric oxide and growth factors that are able to overcome the resorption process.
Conclusions
It is essential to perform a multidimensional evaluation of the patient's asthma control, since the ACT test alone should not be considered reliable because it is a subjective test, since it depends on the patient's responses; however, when correlated with pulmonary function it acquires a greater value, since it is expected to have a normal ACT test with a good pulmonary function, the latter measured with baseline spirometry. Now, in this study, maxillary expansion was added as a therapeutic strategy with the intention of improving nasal breathing, annulling mouth breathing, so that once the expansion was performed, it could be observed that there was no longer a positive bronchodilator response, which was observed at visit zero, suggesting that prior to the expansion the patient could still improve his lung function, which at visits two and three approached optimal values.
According to the results obtained, maxillary expansion had a negative correlation with FEV1, that is, the greater the maxillary compression, the lower the FEV1 value. These data are important because they show that patients with greater upper airway obstruction have decreased lung function, as measured by spirometry.
AFILIACIONES
1Universidad Autónoma de Chihuahua. Chihuahua, Mexico. 2Hospital Infantil de Especialidades de Chihuahua, Hospital Ángeles Chihuahua. Mexico.Conflict of interests: The authors declare that they have no conflict of interests.
REFERENCES
Lucía-Bernal V, Harold M, Herrera-Yudi C, Montoya C. Characteristics dento skeletic with relation to corporal posture in class II malocclusion craniocervical posture in children with class I, II and III skeletal relationships. Pesq Bras Odontoped Clin Integr. 2017;17:1-12. doi:10.4034/PBOCI.2017.171.07.
Soto-Ramos M, Gochicoa-Rangel L, Hinojos-Gallardo L, Hernández-Saldaña R, Baquera-Arteaga M. Evaluación multidimensional del control en el paciente con asma. Aplicaciones clínicas en la toma de decisiones para el tratamiento. Neumol Cir Torax. 2013;72(1):52-61. Available in: https://www.medigraphic.com/cgi-bin/new/resumen.cgi?
|
Table 1: Classification of the degree of obstruction obtained by spirometry. |
|
|
FEV1 % of predicted value |
Obstruction |
|
70-80 |
Mild |
|
60-69 |
Moderate |
|
50-59 |
Moderately severe |
|
35-49 |
Severe |
|
< 35 |
Very severe |
|
Table 2: Predicted percentage values for baseline spirometry at each visit for all patients. |
|||
|
FEV1 % predicted |
Media ± standard deviation |
Minimum |
Maximum |
|
Visit 0 |
86.108 ± 15.92256 |
63.79 |
110.89 |
|
Visit 1 |
85.97467 ± 14.07274 |
62.76 |
110.89 |
|
Visit 2 |
85.85067 ± 17.9075 |
51.44 |
111.83 |
|
Visit 3 |
89.608 ± 14.53569 |
65.33 |
113.10 |
|
Table 3: Correlation between variables with post BD FEV1 and baseline FEV1 values (Pearson correlation). |
||||
|
FEV1 |
%PRED/0 |
%PRED/1 |
%PRED/2 |
%PRED/3 |
|
%PRED/0 |
1.0000 |
|
|
|
|
%PRED/1 |
0.6983 |
1.0000 |
|
|
|
%PRED/2 |
0.7791 |
0.9096 |
1.0000 |
|
|
%PRED/3 |
0.7096 |
0.8445 |
0.9163 |
1.0000 |
|
Table 4: Average percent change per patient post BD. |
||||
|
Patient |
Visit 1 |
Visit 2 |
Visit 3 |
Visit 4 |
|
1 |
5.83 |
1.77 |
1.76 |
3.42 |
|
2 |
0.79 |
1.43 |
6.95 |
1.43 |
|
3 |
0.47 |
7.92 |
11.48 |
4.43 |
|
4 |
2.76 |
8.19 |
1.78 |
0.56 |
|
5 |
6.17 |
4.50 |
2.48 |
6.43 |
|
6 |
8.13 |
11.85 |
2.96 |
19.85 |
|
7 |
11.66 |
11.40 |
4.54 |
5.09 |
|
8 |
5.9 |
7.93 |
8.71 |
7.93 |
|
9 |
1.27 |
1.29 |
2.56 |
1.94 |
|
10 |
4.25 |
8.69 |
4.66 |
6.21 |
|
11 |
3.91 |
3.16 |
1.25 |
5.30 |
|
12 |
3.75 |
17.70 |
4.70 |
8.69 |
|
13 |
3.31 |
2.44 |
3.33 |
2.44 |
|
14 |
26.05 |
21.81 |
15.05 |
13.97 |
|
15 |
3.40 |
0.33 |
5.26 |
2.30 |
|
Table 5: Pearson’s correlation between percent change and maxillary compression post BD. |
|||||||
|
|
|
Compression |
% of change |
||||
|
Anterior |
Posterior |
Visita 0 |
Visita 1 |
Visita 2 |
Visita 3 |
||
|
Compression |
Anterior |
1.000 |
|
|
|
|
|
|
Posterior |
0.7788 |
1.000 |
|
|
|
|
|
|
% of change |
Visit 0 |
-0.0996 |
-0.2330 |
1.000 |
|
|
|
|
Visit 1 |
0.2792 |
0.1928 |
0.7029 |
1.00 |
|
|
|
|
Visit 2 |
-0.1160 |
-0.2868 |
0.5308 |
0.5327 |
1.000 |
|
|
|
Visit 3 |
0.2049 |
-0.1017 |
0.5915 |
0.6795 |
0.2897 |
1.000 |
|


