Descending necrotizing mediastinitis. A 16 years experience from a referral center
Waldo-Hernández, Luis Iván1; Rueda-Villalpando, José Pablo1; Cruz-López, Marco Antonio1; Vázquez-Minero, Juan Carlos1
Waldo-Hernández, Luis Iván1; Rueda-Villalpando, José Pablo1; Cruz-López, Marco Antonio1; Vázquez-Minero, Juan Carlos1
ABSTRACT
KEYWORDS
mediastinitis, abscess, sternotomy, cervicotomy, thoracoscopy.Introduction
Mediastinitis is a severe infection that affects the connective tissue that fills the mediastinum and surrounds the median thoracic organs;1 it is a harsh medical condition of infectious origin. Descending necrotizing mediastinitis (DNM) refers to mediastinal infections originating in the oropharyngeal and cervicofacial regions that spread through the deep planes of the cervical fascia into the mediastinum, causing cellulitis, necrosis, abscesses, and sepsis.2,3 DNM refers to an infection that begins in the oropharyngeal or cervical region, then spreads through the fascial planes in the mediastinum and may or may not spread to the pleural cavity.3-6 Its evolution is rapidly progressive towards tissue necrosis, with high mortality levels (40%) due to sepsis and multiple organ failure without timely and appropriate treatment.4 Surgical treatment plays an essential part in this disease's clinical evolution and prognosis. This study aims to determine the postoperative morbidity and mortality in treatment for DNM, as well as the most prevalent approaches and etiologies in our environment.
Material and methods
This is a retrospective analytical study, conducted in a period from 2006 to 2022, that included all patients diagnosed with DNM treated surgically at the Ismael Cosío Villegas National Institute of Respiratory Diseases (INER) in Mexico City, registered in the database of such procedures of the sub-directorate of surgery. Clinical records were reviewed, including epidemiological data, imaging studies, and available cultures. All patients included were diagnosed based on the criteria of Estrera et al.7 The diagnoses were corroborated by computed tomography and were evaluated based on the classification of Endo et al.8 Patients were excluded when they presented with mediastinitis due to other causes, such as those secondary to esophageal or tracheal perforation secondary to trauma, post-surgical mediastinitis, or those with a diagnosis other than DNM such as superficial or deep neck abscess. Likewise, patients were excluded when retrieving their complete physical or electronic files was impossible.
Results
A total of 51 patients were included, 13 women (25.49%) and 38 men (74.51%); the mean age was 39.19 ± 14.06 years; 13 of them (25.49%) had some comorbidity, the most prevalent being diabetes mellitus and systemic arterial hypertension; 41 patients (80.39%) were classified by tomography as ENDO IIB, nine (17.64%) as ENDO I and one (1.97%) as ENDO IIA. The leading cause and origin of DNM was odontogenic in 28 patients (54.9%), followed by a peritonsillar abscess in 22 patients (43.13%). The average number of days of hospital stay was 22.65 ± 15.61 days. A total of 12 patients (23.52%) underwent surgery by cervicotomy and 39 those (76.48%) with a combined approach, with cervicotomy + median sternotomy being the most common approach in 21 patients (41.17%), followed by cervicotomy + thoracotomy in 16 patients (31.37%). A total of 22 patients (43.13%) needed some surgical reintervention, the most frequent cause being negative pressure therapy replacement in the 11 patients (21.56%) in which it was used, with a mean of 10.78 ± 10.01 days of negative pressure therapy. There were 14 deaths (27.45%); the most common cause was septic shock. The isolated pathogens were multimicrobial, the most common being Klebsiella pneumoniae, streptococcus, E. coli, Serratia marcescens, and Candida. Post-surgical complications occurred in nine patients (17.64%), pulmonary thromboembolism in two patients (3.92%), acute myocardial infarction, acute renal failure, upper gastrointestinal bleeding, supraventricular tachycardia, sternal osteomyelitis, and right cord palsy in one patient, each (1.96%).
Discussion
DNM is a condition originating in a dental or oropharyngeal infection with a rapidly progressive course that can lead to sepsis and often to death. The cause of DNM is distributed as odontogenic (36-47%), pharyngeal or tonsillar (33-45%), cervical (15%), and other head and neck infections (5%).1,4 In our series, the odontogenic origin was the most frequent, with 54.9% of the cases, followed by a peritonsillar abscess.
The most common bacterial flora is an aerobic and anaerobic mix, with β-hemolytic streptococcus being the most commonly isolated.2 Cultures in our series were negative in most cases; however, it was possible to isolate Klebsiella pneumoniae, Streptococcus, E. coli, Serratia marcescens, and Candida, in some cases.
Pearse described the anatomical routes of DNM dissemination in 1983; he was the first to identify this group of patients, which he called "secondary to cervical suppuration".5 The dissemination routes from the neck to the mediastinum are through the pretracheal, paraesophageal, prevertebral, and retropharyngeal spaces, and along the carotid sheath. The main space considered "dangerous" is the retropharyngeal space extending from the skull's base to the mediastinum. This entity's infectious, multimicrobial, predominantly anaerobic nature, association with other comorbidities, and negative intrathoracic pressure ease its spread.9-11
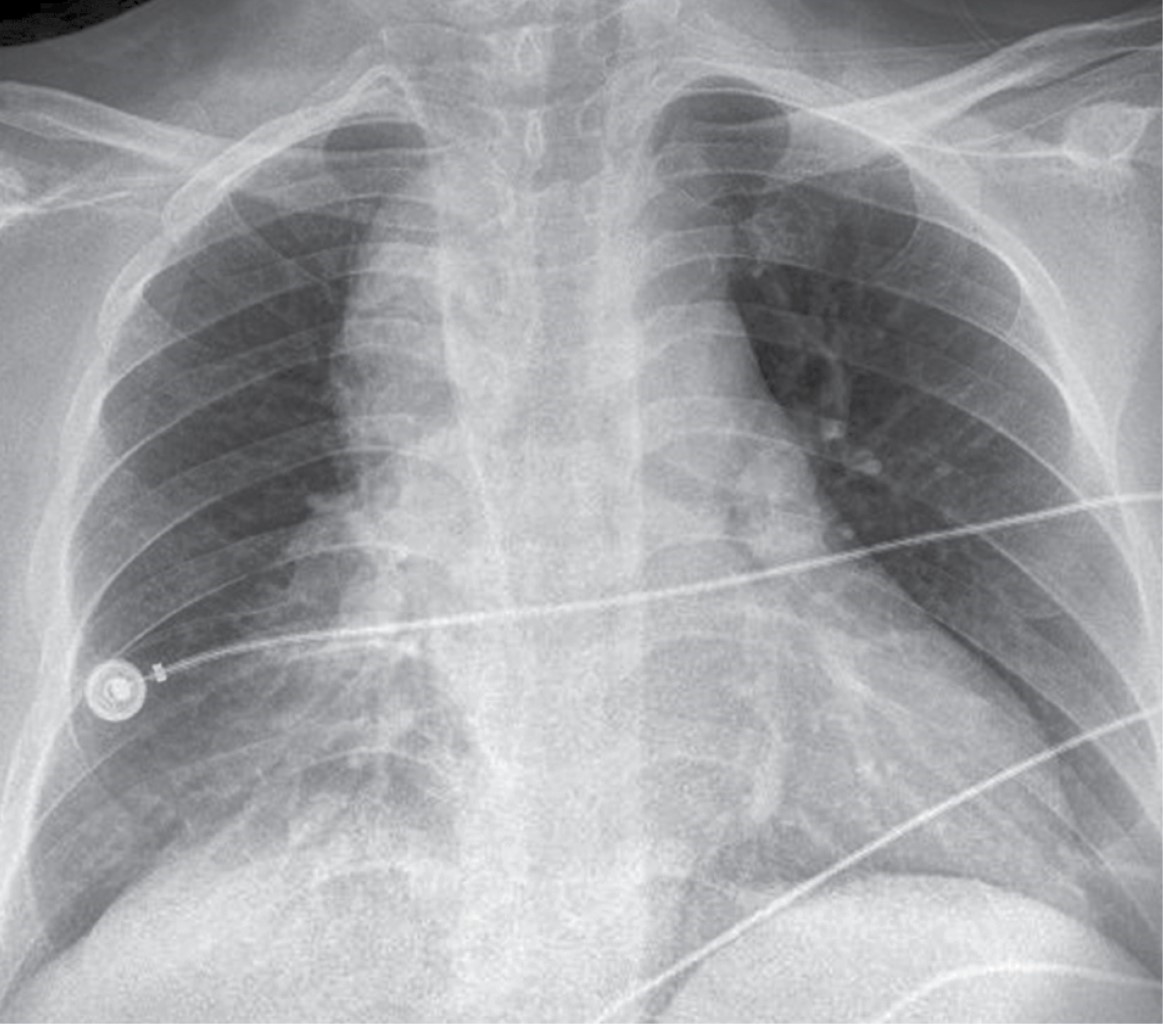
Imaging studies' role is vital in diagnosis, without neglecting a thorough clinical history and physical examination. The main findings in the plain chest x-ray raise the suspicion of DNM and the clinical signs and symptoms of severe infection associated with a history of cervical, dental, or oropharyngeal infection. Said radiological findings can be widening of the mediastinum, pneumomediastinum, mediastinal hydro-aerial levels, anterior displacement of the tracheal air column due to a prevertebral opacity of the soft tissues, enlargement of the cardiac silhouette and loss of the normal lordosis of the cervical spine, as well as unilateral or bilateral pleural effusion.9,10,12 Cervicothoracic computed tomography (CT) should be performed immediately, as CT of the chest and neck can reveal detailed information regarding the extent of the necrosis process and suggests, within the framework of the surgical treatment approach, the best tactic for effective drainage to optimize the best post-surgical outcome for the patient and with it the need for fewer reinterventions.9,10,13-17
In our series, chest radiography continues to be the initial study in all patients with respiratory problems due to its accessibility and quick results (Figure 1); however, chest tomography continues to be the gold standard at our institution for the diagnosis and planning of surgical management in those with mediastinitis (Figure 2).
Management via surgery, and particularly a superior form of mediastinal drainage, is still controversial and ranges from cervical drainage by cervicotomy to a combination of cervical drainage and a thoracic approach using mediastinoscopy, thoracoscopy, thoracotomy, median sternotomy, or a Clamshell incision.1,12 At present, mediastinal and cervical drainage have been particularly benefited with the emergence of negative pressure therapy since the need for aggressive reinterventions and the number of days of hospital stay may be reduced. Our series used negative pressure therapy in 11 patients, with a mean of 10.78 ± 10.01 days of use of the treatment with an average of between one and three changes per patient, with a mean hospital stay of 30.50 ± 19.86 days in the patients with the use of negative pressure therapy versus 20.07 ± 13.66 in whom it was not used. In the pairwise analysis, no statistically significant difference was found in hospital stay days with or without negative pressure therapy with p = 0.132. It should be noted that the historical bias must be considered since, prior to 2016, negative pressure therapy was not employed in our institute, as we did not have it. In the same way and added to the limitation of being a retrospective study, an analysis of a larger sample will be necessary, for which it is unnecessary to resort to the paired analysis of the sample. At the same time, it was recorded that the most significant number of reinterventions was in these patients. However, the procedure to be performed was replacing negative pressure therapy, which is not a major surgical procedure. Although it is performed in the operating room at INER, it is a procedure that can be performed safely in the patient's bed. It will be necessary to expand the sample with future cases to decide if a difference is observed in the days of hospital stay in the patients upon whom it is used versus those cases where it is determined not to use it.
Unquestionably, aggressive surgical drainage is essential for successfully managing DNM,3 since broad-spectrum intravenous antimicrobial therapy is fruitless without effective drainage of the cervical region and mediastinal collections.1 Failure to achieve complete and adequate mediastinal drainage is associated with an increased risk of death.10
Most authors decline the sole use of cervical drainage. Most agree that this approach does not allow complete visualization of the mediastinum and, therefore, adequate excision of necrotic tissue.3 In 1983, Estrera et al. recommended transthoracic drainage for mediastinitis that extends below the fourth thoracic vertebra in the posterior plane since it has been associated with more complications, such as increased pleural empyema.1-4,17,18 Wheatley et al. recommend the combination of cervical and mediastinal drainage before drainage through the subxiphoid approach, along with tracheostomy to secure the airway, since cervical drainage alone has a 70 to 80% failure rate leading to multiple reoperations, prolonged hospital stays and a mortality of almost 40%.1,2,19 Other authors recommend aggressive mediastinal drainage through a standard thoracotomy as the optimal treatment for DNM, regardless of the mediastinal level.16,20-22
In our group of patients, the combined approach was the most used in a total of 39 (76.49%), with cervicotomy combined with median sternotomy being the most used in a total of 21 of them (41.17%), followed by cervicotomy combined with right thoracotomy in 16 patients (31.37%). Median sternotomy also appears to be feasible in DNM type I and IIA but inappropriate in type IIB because access to the posterior and basal compartments of the thoracic cavity is difficult, in addition to being associated with osteomyelitis and sternal dehiscence.3,23,24 In our series, one patient (1.97% of the total and 4.76% of the patients who underwent sternotomy) presented osteomyelitis and sternal dehiscence, requiring chest wall reconstruction with pectoral muscle flaps.
Since the beginning of video-assisted surgery in the 1990s and the extension of its use in thoracic surgery, it has been considered a choice in the treatment of DNM. Roberts et al. reported a case of thoracoscopic drainage as an alternative for the first time in a patient with mediastinal abscesses secondary to esophageal perforation.25 In 2004, Isowa et al. reported successfully managing a patient with DNM via Video Assisted Thoracoscopic Surgery (VATS). In addition, two other groups of authors reported the successful use of VATS in four and nine patients with DNM. Although thoracoscopic drainage has not been wholly described for managing DNM, thoracoscopic exposure allows adequate visualization of the posterior mediastinum with adequate drainage of the collections; likewise, mediastinal collections can be visualized and drained.26-29 Mediastinoscopy-assisted drainage can also be helpful in selected cases.29 In our group of patients, only 3.92% underwent minimally invasive surgery, with adequate postoperative results in both groups. It should be noted that each case must be individualized and consider the degree of mediastinitis and the mediastinal compartments involved to select the surgical approach of choice adequately.
After said management, the hospital's average number of postoperative days was 22.65 ± 15.6. As previously mentioned, there was no statistical difference between the minimally invasive versus open groups and the groups in which negative pressure therapy was or was not used (Figure 3).
Mortality rates remain high, ranging from 12.5 to 37.5% in most recently published series. The leading cause of death is multiple organ failure, for which intensive care unit (ICU) participation is essential. In most published series, long ICU and hospital stays are the rule for patients treated for DNM. The need for a second or even more surgical intervention is also high (33-100%) in most published series, especially after a first attempt to drain the mediastinum through the neck.10
In our series, postoperative complications occurred in nine patients (17.64%), with pulmonary thromboembolism in two of those (3.92%), acute myocardial infarction, acute renal failure, upper gastrointestinal bleeding, supraventricular tachycardia, sternal osteomyelitis, and right cord palsy in one patient, each (1.96%). In addition, there were 14 deaths (27.45%), the most common cause being a septic shock, coinciding with what has been previously reported in the literature. All deaths were recorded in patients who underwent cervicotomy + open approach (sternotomy or thoracotomy), and no deaths were recorded in patients who underwent thoracoscopy and negative pressure therapy; however, a strict relationship between the medical approach and mortality cannot be considered since we have a historical bias. In agreement with what has already been reported in the literature, mortality is associated with the clinical severity of the patient diagnosed with septic shock.
Since there is no standardized algorithm for the surgical management of DNM, the stage and clinical status of the patients should be considered to carefully choose the type of surgery to be performed, as well as the surgical approach that allows the best drainage of the mediastinum and pleural cavities considering the possibilities of each hospital center. Thus, taking into account the data from our review and the current management of patients with DNM at INER, we recommend the following points: 1) a multidisciplinary approach in conjunction with pneumology, intensive care, anesthesiology, infectious diseases, and thoracic surgery; 2) timely diagnosis with CT, early introduction of broad-spectrum antibiotics, and early surgical programming; 3) aggressive surgical drainage, cervicotomy in patients with ENDO I mediastinitis and combined approach (cervicotomy + sternotomy or cervicotomy + VATS versus thoracotomy) in those with ENDO IIA and IIB mediastinitis; 4) the type of thoracic approach (sternotomy, thoracotomy, or VATS) should be decided based on the hospital infrastructure and equipment, as well as the surgeon's experience, as long as complete drainage and debridement of all involved mediastinal spaces are guaranteed.
Conclusions
DNM continues to have impressive morbidity and mortality rates of 30 to 40% or more, almost always attributed to delayed diagnosis and inadequate surgical drainage of the mediastinum. For this reason, DNM needs a multidisciplinary approach based on intensive care unit support, aggressive antibiotic therapy, and said drainage and debridement of the initial infection site and mediastinum, as the prognosis for the disease is poor if proper treatment is not received. The role of surgery is crucial. For a successful result, it is necessary to have extensive knowledge of the cervical and mediastinal anatomy and the routes of the spread of the infection.
The results of our series are similar to those reported in the literature, the approaches described were used according to the availability of resources over time, and both the hospital stay and mortality did not differ from what was reported in the literature.
AFILIACIONES
1Instituto Nacional de Enfermedades Respiratorias Ismael Cosío Villegas. Mexico City, Mexico.Conflict of interests: The authors declare that they have no conflict of interests.
REFERENCES