Tracheal distal third perforation. A case report
Armas-Zárate, Francisco Javier1; Morales-Gómez, José1; Vázquez-Minero, Juan Carlos1; Barrientos-Morales, Edwin Gustavo1
Armas-Zárate, Francisco Javier1; Morales-Gómez, José1; Vázquez-Minero, Juan Carlos1; Barrientos-Morales, Edwin Gustavo1
ABSTRACT
Perforation of the tracheobronchial tree is a potentially life-threatening clinical scenario. The most common causes are iatrogenic perforations. The incidence of this pathology is very low, making appropriate treatment challenging for the surgeon. Bronchoscopy is the gold standard for diagnosis. The most common site of iatrogenic perforations is usually in its proximal third. Treatment should be individualized to each clinical scenario. We present the case of a patient with tracheal perforation in the distal third evidenced by bronchoscopy, with progressive symptoms, who required emergency surgical management with resection and tracheal anastomosis, being its repair challenging due to the anatomical site which is not the most common presented in the literature. With adequate postoperative evolution of the patient. In cases of tracheal perforation and progressive symptomatology, surgical treatment plays a fundamental role.KEYWORDS
perforation of distal third of trachea, thoracic surgery, trachea, case report.Introduction
Perforation of the tracheobronchial tree is a potentially life-threatening clinical scenario.1 The most common causes are penetrating or blunt trauma in 28% and iatrogenic perforations in 58% of cases.2 The incidence of this pathology is often underestimated and underreported.1 Iatrogenic perforations are a rare complication of orotracheal intubation, percutaneous tracheostomy and rigid bronchoscopy, with an incidence of 0.05 to 0.5%.3 Risk factors are divided into mechanical and anatomical. Among the first ones are tracheal instrumentation (rigid bronchoscope, balloon dilatation, among others), emergency orotracheal intubation, female sex and age over 65 years. Among the anatomical factors, congenital abnormalities and tracheal inflammation due to infection or immune pathologies are relevant.1
The clinical presentation of this pathology is nonspecific. Typical findings are subcutaneous emphysema, pneumomediastinum and pneumothorax. Other signs may include respiratory failure, hemoptysis or shock. Its presence will depend on the clinical scenario and the time of presentation may be immediate or delayed.1 A high degree of clinical suspicion is important to establish the diagnosis. Imaging studies, mainly computed tomography (CT) may reveal findings suggestive of tracheal rupture such as pneumomediastinum, subcutaneous emphysema, pneumothorax or tracheal rupture itself.1 The use of imaging studies depends on the stability of the patient and the availability of hospital resources. The gold standard for diagnosis is bronchoscopy. Bronchoscopy helps identify the exact site and size of the rupture; and in some cases treatment, depending on the degree of rupture.1
As for the location of the tracheal rupture, it will depend on the etiological mechanism.1 In rupture of iatrogenic cause, the most common form is the rupture in the membranous portion of the cervical and thoracic segments of the trachea.1 The most commonly used morphological classification for iatrogenic lesions is the one proposed by Cardillo (Table 1).1,4
Treatment should be individualized according to the patient's comorbidities, clinical presentation and anatomy.1,5,6 In grade I and II ruptures, conservative treatment is generally chosen depending on the patient's stability.1,5 While in grade III ruptures, surgical management is usually chosen; however, nowadays, with the use of minimally invasive devices, stent placement can be chosen in some selected cases.1,5
There are no specific guidelines on surgical treatment in patients with tracheal rupture. Traditionally, most experts agree that in rupture larger than 4 cm and in those patients with clinical deterioration surgical treatment is indicated.1,6,7 Most authors also conclude that surgical treatment should be the first choice of treatment for iatrogenic airway injuries.1,6,7
In patients with progressive subcutaneous emphysema, pneumomediastinum, pneumothorax, persistent air leak or lack of lung expansion despite endopleural tube placement, emergency surgical treatment is indicated.1,5 The surgical approach depends on a variety of factors, including location of the tracheal perforation, either in the proximal 2/3 or distal third, including main bronchi; as well as the presence or absence of vascular or other concomitant organ injury. For any surgical approach it is important to gain adequate exposure to examine adjacent organs for damage.1,7
If the perforation involves the proximal 2/3 of the trachea, the repair can be via the cervical route.1,5 If the middle third is involved, the incision can be extended in a T-shape, with opening of the sternal manubrium.1,5,7 Perforations involving the distal 1/3 of the trachea and the carina or any of the main bronchi can be approached via right thoracotomy, with a median sternotomy being an option.1,5,7
The most relevant prognostic factors for mortality in these patients are the extent of tracheal perforation (greater than 4.5 cm) and the development of mediastinitis.8
We report a challenging case due to the site where the tracheal stenosis was located (distal third), which is the least common and due to the low frequency and the scarce availability of guidelines on the subject, many authors recommend the approach according to the experience of the surgeon in charge. In addition, the context in which the perforation occurs, with limited ventilation and the impossibility of having a Y stent, as a possibility of endoscopic management, meant that this case had immediate surgical management.
Case presentation
A 36-year-old woman. History of prolonged orotracheal intubation for 60 days, without tracheostomy, 10 years ago secondary to hemorrhagic shock due to ectopic pregnancy that required left oophorectomy. Prolonged hospitalization for hospital pneumonia and critical patient myopathy, with hospital discharge 14 months later. Subsequently with progressive dyspnea and stridor. She was evaluated two years later by thoracic surgery who diagnosed tracheal stenosis and performed fibrobronchoscopy and mechanical tracheal dilatation three times in a period of one year.
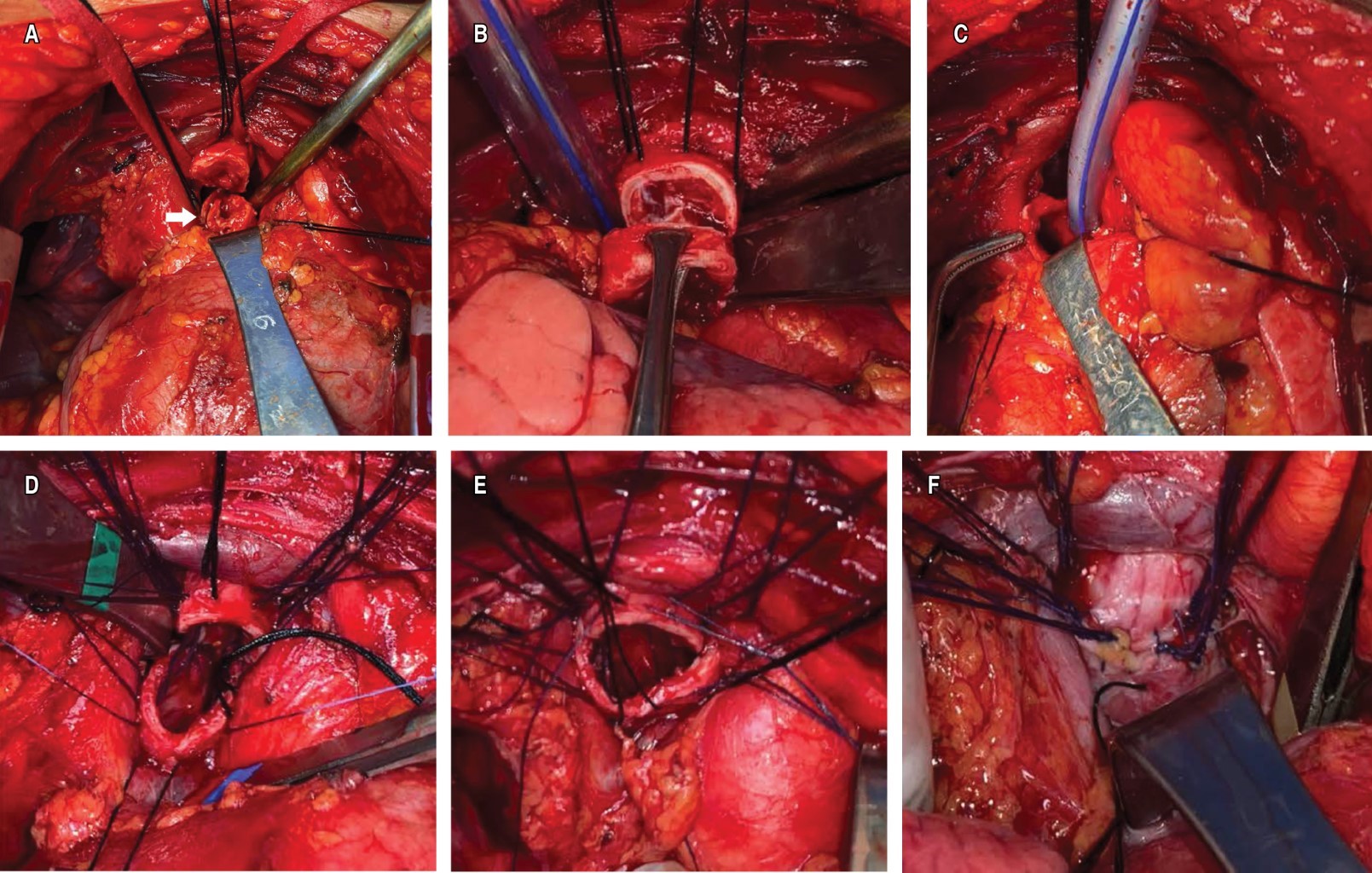
Subsequently, she was referred to a tertiary hospital where she was followed up conservatively. A year ago, she presented with progressive dyspnea and stridor, for which she was referred to the Instituto Nacional de Enfermedades Respiratorias (INER) Ismael Cosío Villegas, Mexico City. A revision fibrobronchoscopy was scheduled, which showed tracheal stenosis to nine tracheal rings of the vocal cords, 1.5 cm long, with four free tracheal rings to the main carina; hydrostatic balloon dilatation was performed, achieving a post-dilatation lumen of 80%. Due to recurrence of symptoms, the patient underwent a new fibrobronchoscopy one month later. It was decided to approach with rigid bronchoscopy to dilate the stenosis and a granuloma was observed at the end of the stenosis, which was resected with biopsy forceps, after which a perforation was observed in the right lateral face of the trachea of approximately 0.5 cm to a main carina ring. The patient started with progressive subcutaneous emphysema, with difficulty in mechanical ventilation, so it was decided to perform a median sternotomy to repair the perforation. She was not considered a candidate for endoscopic management with stent, due to the proximity of the perforation to the carina and the need for a Y-stent, which is not available at the institute. Tracheal perforation was found at the level of the eleventh tracheal ring of 0.5 cm in length, so it was decided to perform resection of the stricture site from the tenth to the twelfth tracheal ring, with terminoterminal anastomosis between the ninth and thirteenth tracheal ring without tension (Figure 1). Associated esophageal perforation was ruled out with transoperative endoscopy. She passed the postoperative period without complications. Endopleural and mediastinal probes were removed on the fifth day. Hospital discharge was on the seventh day. No respiratory symptoms at six months' post-surgery, evidenced by control spirometry, within normal parameters, and clinically without stridor and with adequate phonation.
Discussion
Tracheobronchial tree perforation is a medical-surgical emergency that requires a rapid response from the surgical and anesthetic team to achieve adequate patient outcomes.
The gold standard for diagnosis is bronchoscopy. In this case the perforation occurred during tracheal instrumentation, so the diagnosis was made at the time of the procedure.
Signs and symptoms may vary in the presentation of tracheal perforation due to the time and form of presentation. In our case, the signs were immediate (subcutaneous emphysema in the neck, thorax and abdomen, in addition to leakage in mechanical ventilation with difficulty in ventilation) with a rapid evolution, which led to emergency surgical management.
Depending on the time of evolution, site of perforation and experience of the surgical team, different approaches can be performed. In the literature, right thoracotomy is proposed as the approach of choice for distal third perforations. In this case, a median sternotomy approach was chosen, since rapidly progressive symptomatology was presented, and therefore it was considered that the sternotomy had a better field of exposure for surgical resolution.
The type of repair will depend mainly on the extent and conditions of the particular patient. In our case it was a grade IIIA Cardillo perforation (Table 1), so it was not considered for endoscopic treatment. The repair was with resection and terminoterminal anastomosis, since the underlying pathology was a benign post-intubation tracheal stenosis, and when the perforation was present within the segment with stenosis, it was decided to resect the entire affected part.
In this case she was not considered a candidate for endoscopic management, due to the proximity of the perforation to the tracheal carina, which would require a Y-stent, which is not available at the institute; however, if available, it is a viable option. The patient had no risk factors for short-term mortality. The good functional status, perforation with short extension (0.5 cm) and rapid treatment contributed to the adequate evolution.
The approach to complex tracheal stenosis will always be recommended in hospitals with trained and experienced thoracic surgeons in the definitive treatment and resolution of possible complications such as tracheal perforation.
Conclusions
The approach and treatment of the patient presenting with a tracheobronchial tree perforation depends on multiple patient factors and the hospital environment. A multidisciplinary team with experience in the appropriate management of these patients is recommended. Adequate airway control and, regardless of the approach, adequate repair of the perforation is essential, which leads to better patient survival rates and lower morbidity and mortality.
AFILIACIONES
1Instituto Nacional de Enfermedades Respiratorias Ismael Cosío Villegas. Mexico City, Mexico.Conflict of interests: the authors declare that they have no conflict of interests.
REFERENCES
|
Table 1: Morphological classification of Cardillo’s tracheal rupture.1,4 |
|
|
Grade |
|
|
I |
Mucosal or submucosal rupture without mediastinal emphysema or esophageal perforation |
|
II |
Rupture extending into the muscle wall with subcutaneous or mediastinal emphysema without esophageal perforation or mediastinitis |
|
IIIA |
Complete rupture with mediastinal or esophageal soft tissue herniation without esophageal perforation or mediastinitis |
|
IIIB |
Any rupture with esophageal perforation or mediastinitis |


