Esophageal balloon in ECMO: clinical case report
López-Zamora, Venus Nefte1; Maldonado-Beltrán, Ismael1; Lugo-Goytia, Gustavo1; Hernández-Cárdenas, Carmen Margarita1
López-Zamora, Venus Nefte1; Maldonado-Beltrán, Ismael1; Lugo-Goytia, Gustavo1; Hernández-Cárdenas, Carmen Margarita1
ABSTRACT
Severe respiratory distress syndrome, which does not respond to conventional strategies, benefits from veno-venous extracorporeal membrane oxygenation therapy. This bridging therapy can be complemented with lung ultra-protection maneuvers. Transpulmonary pressure may help reduce the risk of ventilator-induced lung injury due to atelectrauma. However, its benefit remains to be established. We present the case of a 34-year-old man with severe acute respiratory failure syndrome receiving veno-venous extracorporeal membrane oxygenation therapy and ultrapulmonary protective ventilation, with positive end-expiratory pressure titration by transpulmonary pressure. Veno-venous extracorporeal membrane oxygenation was successfully decannulated after adequate resolution of the acute respiratory distress syndrome. In this case, it was possible to observe that a ventilation strategy that uses esophageal pressures to estimate transpulmonary pressure significantly improves oxygenation, compliance, and minimizes ventilation-induced lung injury.KEYWORDS
COVID-19, acute respiratory distress syndrome, extracorporeal membrane oxygenation, esophageal balloon.Introduction
Acute respiratory distress syndrome (ARDS) has a high mortality rate (35-46%).1,2 Severe ARDS, with PaO2/FiO2 of 80 mmHg and no response to conventional mechanical ventilation (MV), requires extracorporeal membrane oxygenation (ECMO) as rescue therapy.1,3 ECMO therapy provides oxygenation and ventilation,2 allowing the lungs to rest and recover from respiratory failure while minimizing ventilator-induced lung injury (VILI).1-3
Ultraprotective lung ventilation is a strategy that achieves lower airway pressures and tidal volume (TV) than the current standard. This maneuver sets several parameters: low tidal volume (0.5-6 mL/kg/min), high positive end-expiratory pressure (PEEP) (10 to 15 cmH2O), low plateau pressure (< 25 cmH2O),1,2 limited respiratory rate,2,3 inspiratory time of one to two seconds, low inspiratory pressure (< 15 cmH2O), and FiO2 less than 60%.2,3
It is feasible to adjust ventilator settings based on transpulmonary pressure (TPP) measurements, which can improve oxygenation and reduce VILI secondary to high pressures and volumes during inspiration and low pressures and volumes during expiration.1-3 However, there are few studies on ECMO where the impact of PEEP adjustment based on TPP is determined.3 Transpulmonary pressure measurement is based on esophageal manometry. The aim of this work is to present a case of TPP measurement with esophageal balloon achieving control of VILI in a patient with severe ARDS.
Case presentation
A 34-year-old Mexican male with a history of smoking and cocaine abuse, with no history of SARS-CoV-2 vaccination, developed asthenia, hyperthermia and dry cough in February 2022. First treated on an outpatient basis (paracetamol, supplemental oxygen, antibiotics, anticoagulant, steroids, tocilizumab and inhaled bronchodilator), his clinical picture worsened 35 days after symptom onset and he was admitted to the intensive care unit with arterial saturation of 60% and confirmatory COVID-19 test. Advanced airway management was performed, with subsequent recruitment maneuver and PEEP titration for distensibility. However, pulmonary protection goals were not achieved. Due to severe ARDS, the patient was placed in prone position and antibiotic therapy was started due to suspicion of bacterial pneumonia.
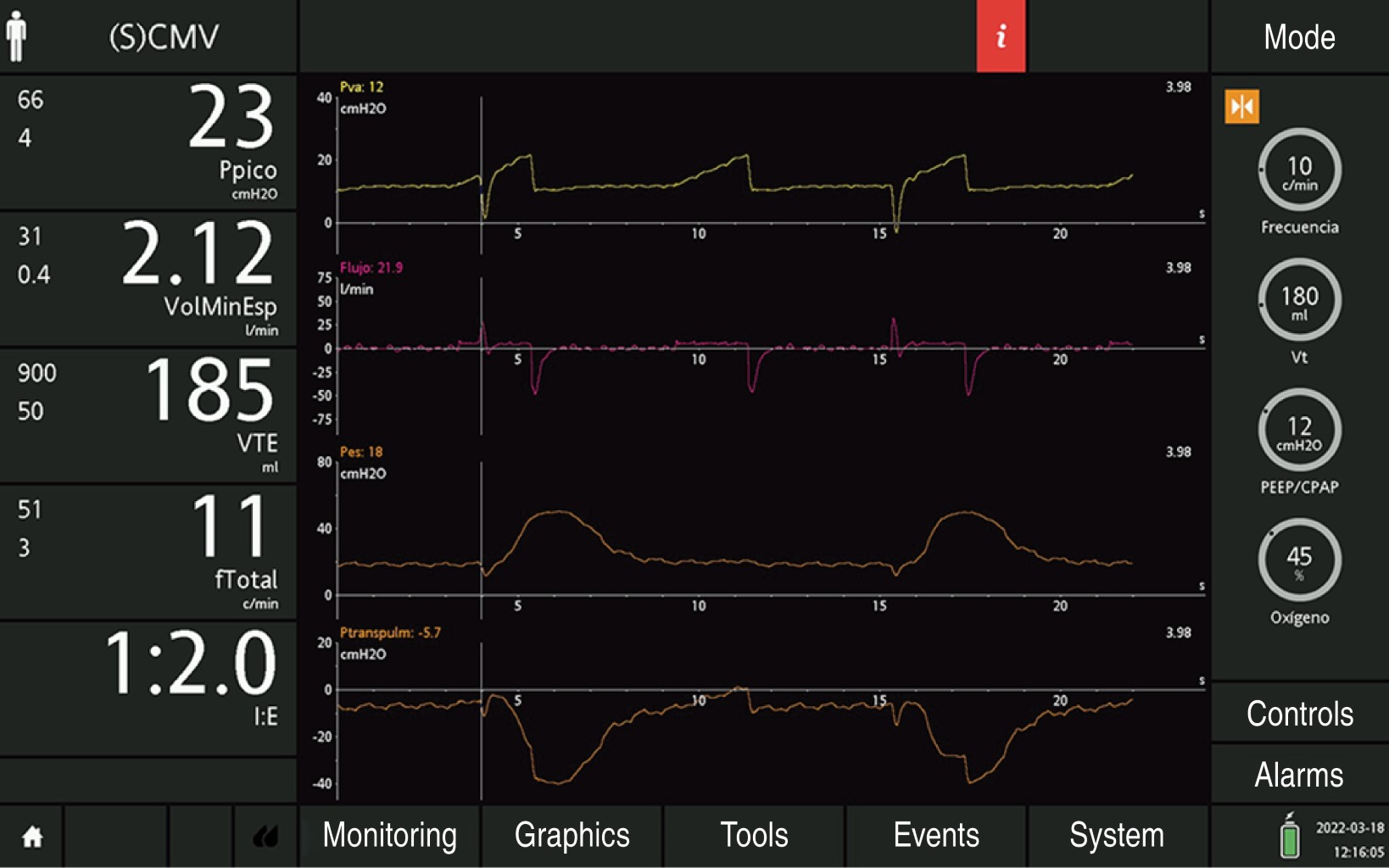
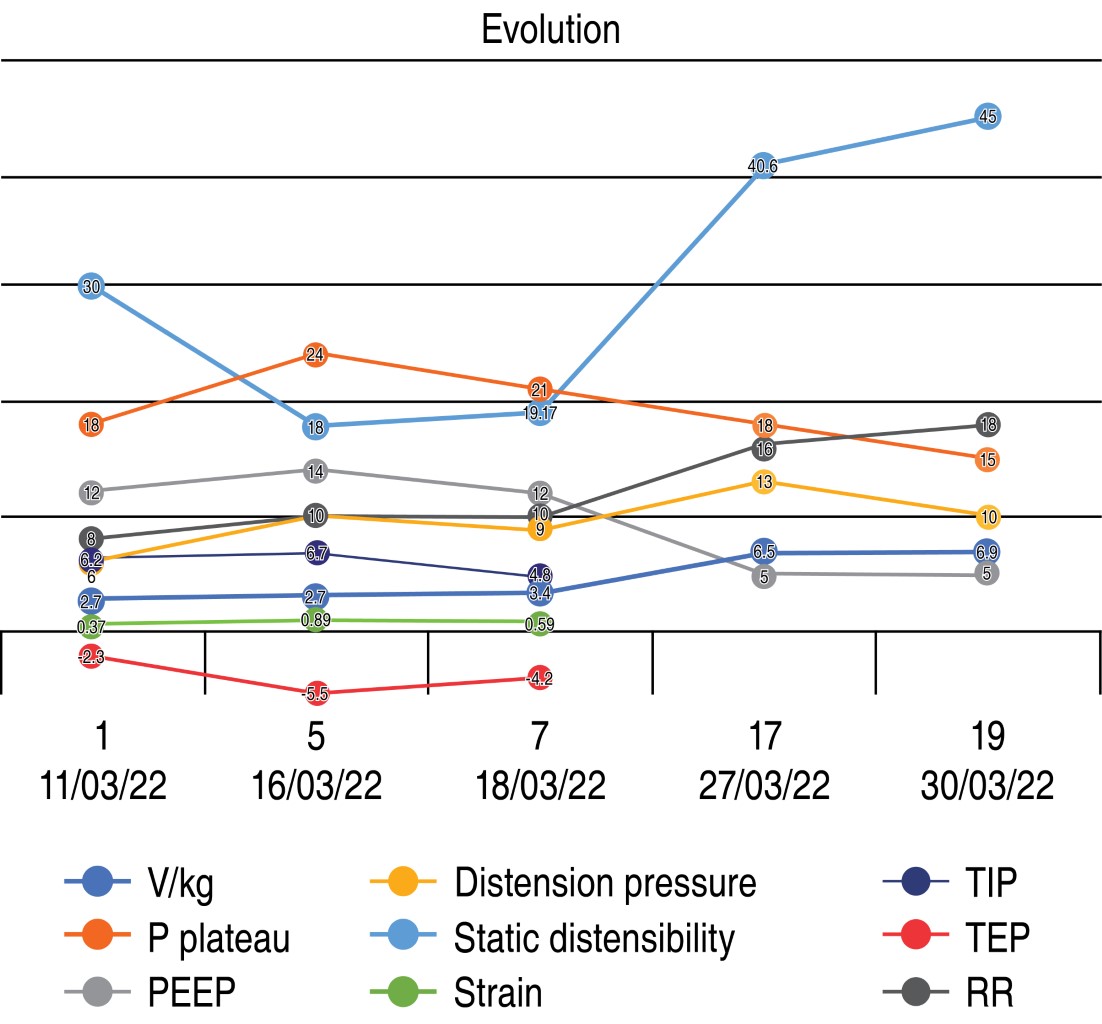
Despite pharmacological adjustments (analgesia, sedation and neuromuscular blockade), his poor tolerance to PEEP and persistent refractory hypoxemia (PaO2/FiO2 64.9 mmHg), he was considered a candidate for venovenous ECMO (VV ECMO). With SOFA of 10 points, 50% mortality, MuLBSTA score 12 points, 15.99% mortality at 90 days, RESP score six points, risk classification I and hospital survival of 92%. An esophageal balloon was placed and ventilation settings were established with pulmonary ultraprotection. Due to the high requirement for intravenous sedation, inhalation sedation with sevoflurane was administered to achieve deep sedation (bispectral index 34-47) and patient-ventilator synchrony. On day nine, patient-ventilator asynchrony was observed due to secondary false triggering by synglot (Figure 1), so proton pump inhibitors were started and sedoanalgesia was adjusted. On day 17 ECMO support was reduced and MV parameters were adjusted, achieving pulmonary protection goals. Ineffective efforts were determined using esophageal balloon. On day 19 the resolution of ARDS allowed ECMO withdrawal and maintenance of lung protection goals; however, with deterioration 48 hours later due to ventilator-associated pneumonia. A titration procedure with esophageal balloon support and electrical impedance tomography was performed, with adequate resolution at 72 hours. On day 25 rehabilitation was started after removal of neuromuscular blockade and sedation with progressive withdrawal of analgesia. On day 27 tracheostomy was performed, allowing ventilatory progression on day 32, according to TIPS protocol. A positive swallow test was performed on day 42, followed by successful tracheostomy decannulation on day 44 (Figure 2).
Discussion
ARDS has a high mortality rate (35 to 46%).1,2 Mortality and ventilator days' increase with severity.2 ARDS is characterized by severely impaired gas exchange. Hypoxemia is mainly due to intrapulmonary shunt, while increased alveolar dead space accounts for impaired CO2 clearance. Patients with severe ARDS, with PaFi less than 80 mmHg, unresponsive to conventional mechanical ventilation are considered candidates for VV ECMO as rescue therapy.1,3 The rationale is that extracorporeal gas exchange allows the use of lung protective ventilator settings, which minimizes VILI.1-3 While none of the guidelines (REVA, CESAR, ELSO or EOLIA)2,3 have yet defined the ultra-protection configuration in the ventilator, there is no agreement on its benefit.1-3 Patients with severe ARDS are more likely to present with VILI. The predominant mechanisms by which VILI occurs include alveolar overdistension (volutrauma), barotrauma, atelectotrauma and inflammation (biotrauma).1-3 Lung protective ventilation strategies are the current standard of care for patients with ARDS that provide adequate ventilation requirements and minimize VILI. Ultra-lung protective goals include the following settings: low tidal volume (0.5-6 mL/kg/min), high PEEP (10 to 15 cmH2O), plateau pressure limitation (< 25 cmH2O),1,2 limited respiratory rate,2,3 inspiratory time of one to two seconds, inspiratory pressure < 15 cmH2O, and FiO2 below 60%, ideally 30%.2,3 The optimal strategy for assessing and preventing VILI in ARDS is controversial. In patients with severe ARDS with VV ECMO support the optimal mechanical ventilation strategy is unclear.
Measurement of TPP is based on esophageal manometry. Harmful forces causing alveolar overdistension correlate directly with peak inspiratory TPP, and trauma from recurrent alveolar collapse and reopening correlates with minimal end-expiratory TPP.4 Therefore, knowledge of end-inspiratory and end-expiratory TPP, rather than just airway pressure, could allow customization of mechanical ventilator settings for each patient to minimize both causes of VILI. The use of the esophageal balloon is an appropriate strategy to assess lung function with a personalized approach.3
Grasso et al.5 measured TPP in patients with severe ARDS and increased PEEP until TPP was 25 cmH2O. Of the patients, 50% responded to increased airway pressure and did not require VV ECMO.
In 2019 Zee et al.6 described eight patients with severe ARDS and indication for VV ECMO, according to the EOLIA trial. They estimated TPP with an esophageal balloon catheter and aimed for a TPP ≤ 25 cmH2O. The TPP-guided open lung concept resulted in an increased PaO2/FiO2 ratio and none of the patients required VV ECMO, with a reduction in mortality of 11%.6
In a single-center prospective randomized controlled trial in patients with VV ECMO, 104 patients were randomized to the transpulmonary pressure-guided ventilation or lung rest strategy group.1 The proportion of patients successfully weaned from VV ECMO in the transpulmonary pressure-guided group was significantly higher than in the lung rest group (71.2 vs 48.0%; p = 0.017).1
Limiting tidal volumes to maintain end-inspiratory TPP below 25 cmH2O has been shown to improve oxygenation and compliance; on the other hand, end-expiratory TPP between 0 and 10 cmH2O prevents atelectasis.7 As a strategy to maintain convective ventilation for alveolar nitrogen removal and avoid alveolar collapse during ECMO, a high PEEP level should be combined with a very low tidal volume.8,9 This stabilizes lung morphology improving lung function and limiting hemodynamic impact.1,3 However, it is still an uncertain strategy in ECMO.1 In our patient, adjusting ventilator settings based on transpulmonary pressure measurements by esophageal manometry prevented ventilator-induced lung injury and allowed early identification of asynchrony, which allowed successful weaning from VV ECMO.
Conclusions
A ventilation strategy using esophageal pressures to estimate transpulmonary pressure significantly improves oxygenation, distensibility and minimizes VILI. We present a successful case of a patient with severe ARDS on VV ECMO and transpulmonary pressure monitoring with the use of esophageal balloon catheters that allow finding a PEEP value that could maintain oxygenation, while preventing lung injury due to repeated alveolar collapse or overdistension.
AFILIACIONES
1Instituto Nacional de Enfermedades Respiratorias Ismael Cosío Villegas. Mexico City, Mexico.Conflict of interests: the authors declare that they have no conflict of interests.
REFERENCES