Focused transesophageal echocardiography to guide double cannulation in venous-venous ECMO during COVID-19 pandemic
Manzur-Sandoval, Daniel1; García-Cruz, Edgar1; Navarro-Martínez, Daniel Alejandro1; Mier y Terán-Morales, Elisa1
Manzur-Sandoval, Daniel1; García-Cruz, Edgar1; Navarro-Martínez, Daniel Alejandro1; Mier y Terán-Morales, Elisa1
ABSTRACT
The usage of transesophageal echocardiogram as a guide for positioning cannulas of extracorporeal membrane oxygenation, has become controversial. While extracorporeal membrane oxygenation is largely recommended as a rescue maneuver in patients with COVID-19 who undergo acute respiratory distress syndrome, the usage of transesophageal echocardiogram is not recommended by the American Society of Echocardiography due to the high transmission rate from this pathogen. However, transthoracic echocardiogram has important limitations in patients with acute respiratory distress syndrome that make transesophageal echocardiogram necessary under such circumstances. In this case report, we review the case of a 38-year-old male with severe acute respiratory distress syndrome due to COVID-19 that was started on venous-venous extracorporeal membrane oxygenation. We also describe how the extracorporeal membrane oxygenation team of our institution performs a low-risk focused transesophageal echocardiogram-guided venous-venous extracorporeal membrane oxygenation cannulation adapting to the World Health Organization recommendations on personal protective equipment and the Extracorporeal Life Support Organization recommendations on extracorporeal membrane oxygenation cannulation.KEYWORDS
extracorporeal membrane oxygenation, transesophageal echocardiogram, COVID-19, cannulation, acute respiratory distress syndrome.Introduction
More than two years have passed since the onset of the COVID-19 disease outbreak. At this point in the pandemic, the number of critically ill patients is declining; however, information about diagnostic protocols and management remains scarce.
An example of this deficiency is the controversial use of transesophageal echocardiography (TEE) in critically ill patients with COVID-19 to guide extracorporeal membrane oxygenation (ECMO) cannulation. Undoubtedly, TEE is a support tool for intensivists to be able to set management goals within the intensive care unit. Furthermore, it has been shown to be the ideal modality for patients with COVID-19 who are hemodynamically unstable or who require serial pulmonary assessments, support during cardiac arrest resuscitation, and guidance during venous-venous extracorporeal membrane oxygenation (VV ECMO) cannulation.1 However, some societies such as the American Society of Echocardiography have mentioned that despite the usefulness of TEE in the management and evaluation of critically ill patients with COVID-19, this imaging modality represents an increased risk of viral transmission. This is why the use of TEE should be considered with caution.2
At the Instituto Nacional de Cardiología "Ignacio Chávez" in Mexico City, TEE is preferred over transthoracic echocardiography (TTE) for VV ECMO cannulation. During the last year, a case series of 13 patients in which TEE was used to guide successful VV ECMO cannulation was published.3
In this case report we explain the protocol that intensive care physicians at the institute follow during TEE-guided placement of extracorporeal membrane oxygenation cannulae.
Case presentation
A 38-year-old man with acute respiratory distress syndrome (ARDS) secondary to COVID-19 infection refractory to conventional treatment and ventilation in the prone position, for which ventricular support with VV ECMO was initiated. This was done following the protocol and recommendations of the World Health Organization (WHO) regarding personal protective equipment (PPE) and adapting the recommendations for TEE-guided ECMO cannulation of the Extracorporeal Life Support Organization (ELSO).4 Based on this, the ECMO team was composed of intensivists specialized in critical echocardiography trained with the skills to guide real-time ECMO cannulation in order to limit microdroplet exposure time and, likewise, ECMO-associated complications such as bleeding, infection, malpositioning and recirculation.
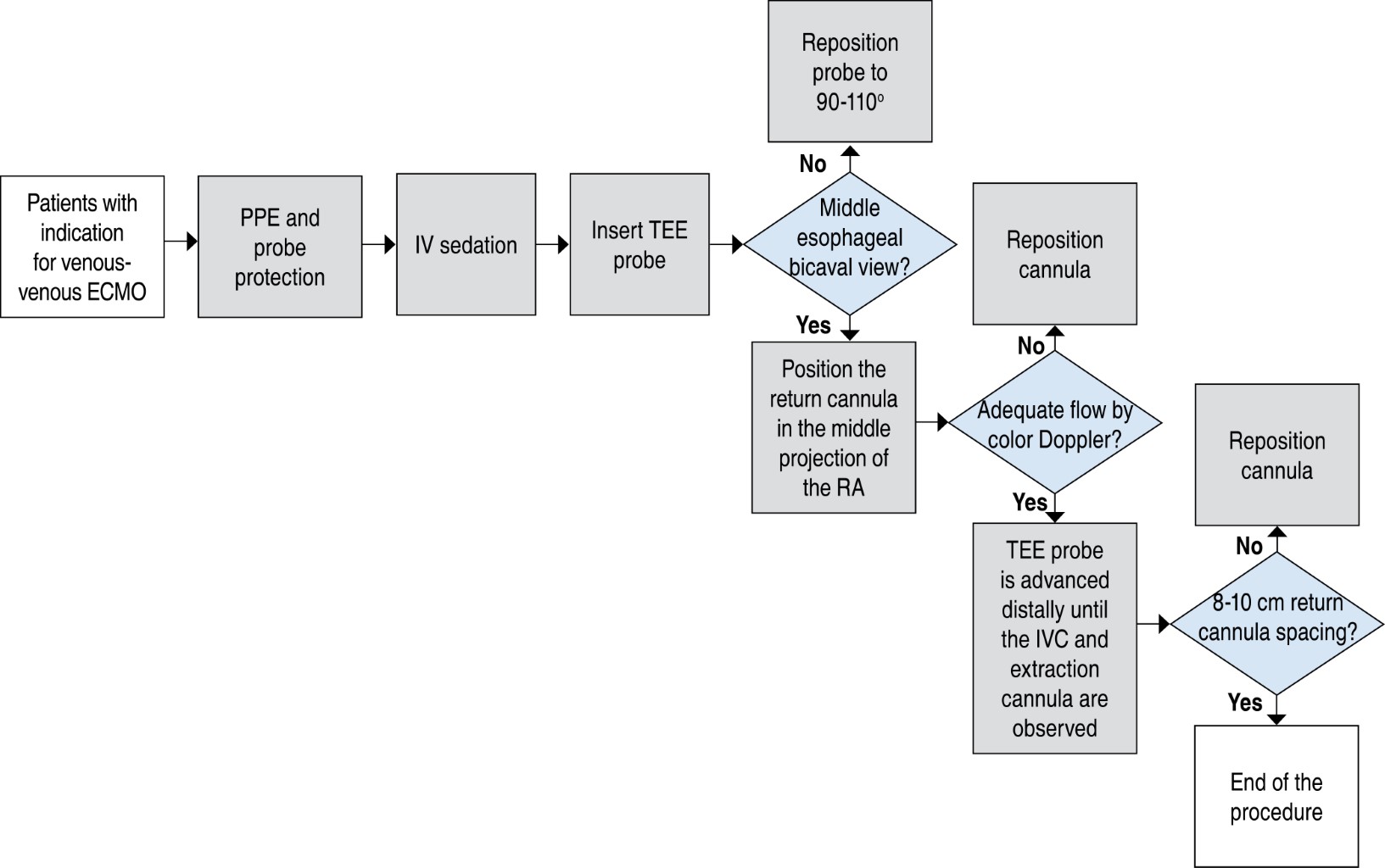
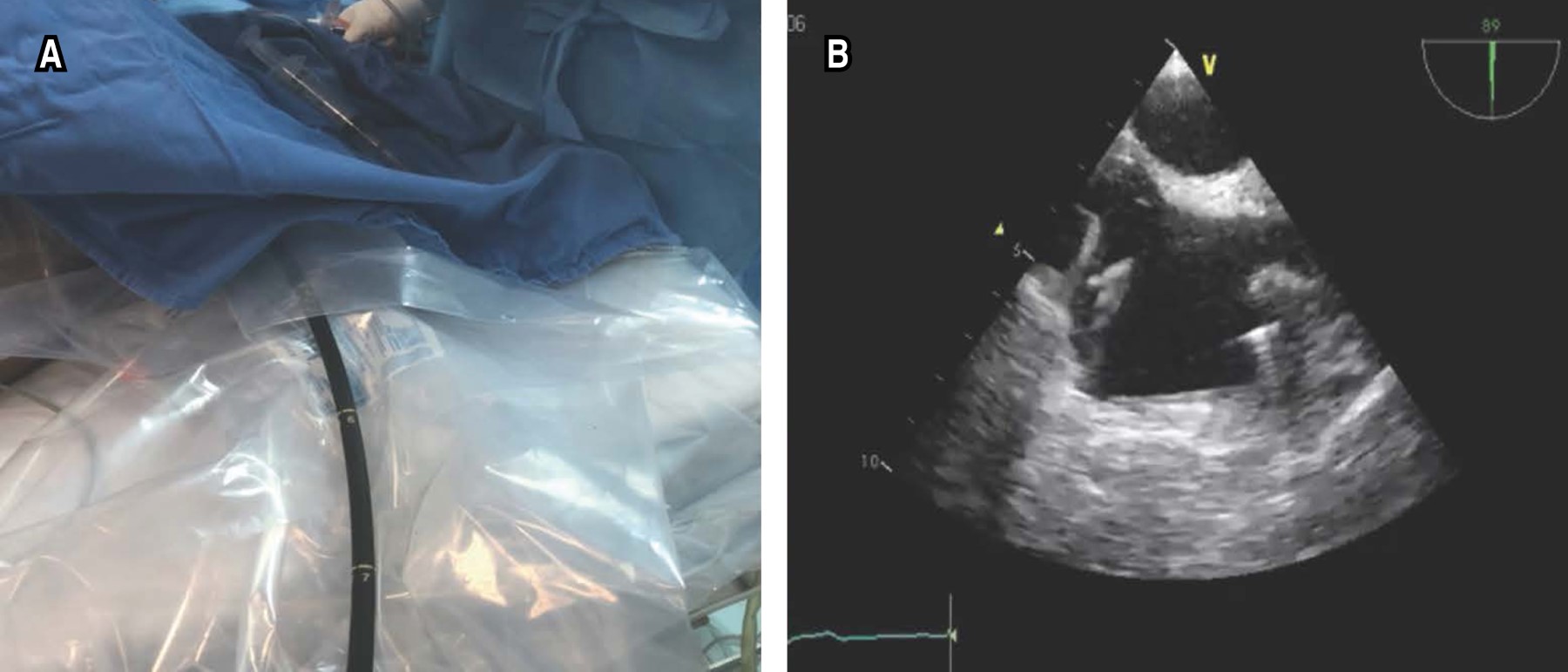
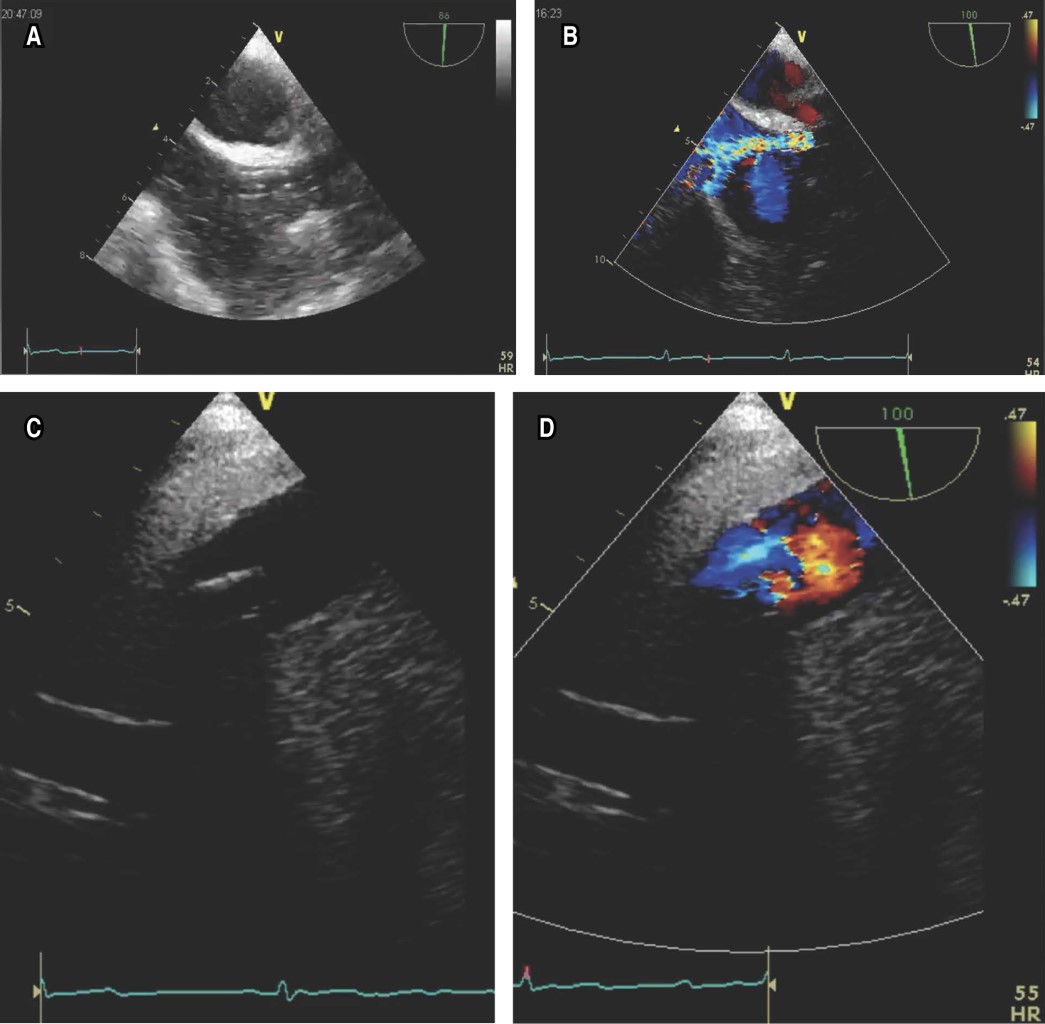
As the first step of the flowchart (Figure 1), all personnel must have adequate PPE and protect the TEE probe (Figure 2A). After intravenous sedation, the TEE probe is inserted, being the projection selected to guide the procedure the mid esophageal bicaval 90-110 degree view (Figure 2B), where we can guide in real time the correct positioning of the return (jugular) cannula (Figure 3A), which should be placed in the mid portion of the right atrium in the direction of the tricuspid valve. Adequate flow can be assessed by color Doppler (Figure 3B). The TEE probe with the same degree of angulation is advanced distally toward the esophagus to observe the inferior vena cava and the extraction cannula (femoral) which should be separated 8 to 10 cm from the return cannula (Figure 3C and D); this limits suction and recirculation phenomena.
Discussion
The ELSO, WHO and the Surviving Sepsis Campaign Guidelines recommend considering ECMO in specialized centers as a rescue maneuver in patients with COVID-19, acute respiratory distress syndrome and severe hypoxemia despite optimal medical treatment.5 The reported hospital mortality in patients with COVID-19 receiving ECMO is 37.1%.6 Given the high rate of transmission of this pathogen through airborne particles, societies such as the American Society of Echocardiography2 do not recommend some procedures such as transesophageal echocardiography as a first diagnostic approach. The ELSO group suggests that VV ECMO and cannulation should be guided by TEE to ensure correct positioning of the cannulae.4 On the other hand, in cases where there is biventricular dysfunction, the use of VV ECMO will be insufficient to improve the patient's clinical condition. These patients can be adequately selected by TTE; in addition, there are reports of the use of TTE as a tool to guide VV ECMO cannulation;7 however, patients with ARDS often have a poor acoustic window due to positive pressure during mechanical ventilation, prone decubitus and/or obesity, so image quality is not always optimal; TEE is necessary in these scenarios.
Conclusions
Severe forms of COVID-19 infection will continue to be a frequent scenario in intensive care units in the coming years, making the integration of multidisciplinary teams capable of providing mechanical respiratory and circulatory support mandatory. Therefore, any imaging evaluation should be done in a "focused" manner to minimize staff exposure to infectious particles, while providing the best evidence-based management of critically ill patients.
AFILIACIONES
1Instituto Nacional de Cardiología "Ignacio Chávez", Mexico City, Mexico.Conflict of interests: the authors declare that they have no conflict of interests.
REFERENCES
Kirkpatrick JN, Mitchell C, Taub C, Kort S, Hung J, Swaminathan M. ASE statement on protection of patients and echocardiography service providers during the 2019 novel coronavirus outbreak: Endorsed by the American College of Cardiology. J Am Soc Echocardiogr. 2020;33(6):648-653. Available in: https://doi.org/10.1016/j.echo.2020.04.001
Moore B, Morgan N, Selzman C, Zimmerman J. Successful use of limited transthoracic echocardiography to guide veno-venous extracorporeal membrane oxygenator placement in a patient with coronavirus disease 2019. J Cardiothorac Vasc Anesth. 2020;34(12):3491-3493. Available in: https://doi.org/10.1053/j.jvca.2020.04.047