Institutional robotic assisted thoracic surgery program: mandatory necessity
Hernández-Ramírez, Israel1; Espinoza-Mercado, Fernando1; Corona-Perezgrovas, Miguel Ángel1; Rivera-Navarrete, Eric1
Hernández-Ramírez, Israel1; Espinoza-Mercado, Fernando1; Corona-Perezgrovas, Miguel Ángel1; Rivera-Navarrete, Eric1
ABSTRACT
KEYWORDS
.Thoracic surgery is a thriving area in the surgical field in our country; it has become a specialty that has progressively acquired its own personality, with a well-established professional pathway and well-defined competencies for the optimal surgical care of non-cardiac thoracic pathology. As it has happened with all other medical specialties, the development of technology and scientific advances in the understanding and treatment of diseases, has forced the increasingly less invasive surgical treatment of thoracic pathology; this undoubtedly has to go hand in hand with specific training in minimally invasive approaches, in which the same principles and results as conventional surgery are preserved, always seeking to improve them.
Video-assisted thoracic surgery (VATS) is the gold standard in a wide variety of procedures, which favors a faster postoperative recovery, thus reducing hospital costs related to time in the operating room, amount of drugs used, days of hospital stay and lower rate of infectious complications. Worldwide, the emergence of robotic platforms for performing surgeries in various fields has raised a wide variety of questions about the cost-benefit of using this sophisticated equipment. In the field of thoracic surgery, robotic-assisted thoracic surgery (formerly abbreviated as RATS) has been reported since the early 2000's, and the first report of robotic-assisted lung lobectomy as a treatment for lung cancer was published in 2002.1 In that regard, definitions for robotic thoracic procedures have changed, as the Clinical Guidelines Committee of the American Association for Thoracic Surgeons (AATS) created a working group with the purpose of unifying a system of nomenclature and definitions to standardize robotic-assisted thoracic procedures.2 A four-letter system was proposed, where the letter R refers to a robotic approach, P when only ports are used, or A if assisted (through a utility or working port); the next part, is the abbreviation of the procedures performed and the final element is the number of robotic arms. Under this system, for example, a robotic lobectomy can be described as RPL (3 or 4) or as RAL (3 or 4).
In Mexico, there are reports of the first robotic thoracic surgeries since 2017 and, although in some specialties its use has become popular, thorax remains a pending task, which depends on multiple factors, not only on training and certification in its use for thoracic surgeons. The final decision to acquire a robotic system is not made by the end users (patients), but by institutions or hospitals that, for the sake of competitiveness and prestige, seek to attract surgeons and patients "seduced" by the benefits of sophisticated, state-of-the-art technology. High equipment acquisition and maintenance costs, limited availability of supplies and still long operating times are important factors that have limited its use; recent studies have shown that a rational and multidisciplinary use of equipment together with optimal postoperative management can improve the cost-benefit relation.3 It should be mentioned that the benefits in the use of robotic systems cannot be fully achieved until sufficient efficiency in their use is achieved, which according to initial reports could reach between 150 and 250 procedures to feel comfortable in their use,4 a very high and prohibitive figure for most; Melfi et al. and Gharagozloo recommend at least 20 cases of robotic thoracic surgery to acquire sufficient skills, while Jang et al. report that the learning curve for a robotic lobectomy is less than that required for a VATS lobectomy.5
Although to date there are still no clear differences between VATS and RATS, some benefits have been recognized with the use of robotic systems. These benefits include: clearer, three-dimensional visualization of anatomical structures, finer and more controlled movements within small spaces, wider range of motion with robotic instruments, as well as better ergonomics for the surgeon while working at the console.6 Several meta-analyses have been conducted to try to determine the benefit of one approach over the other; to date, most conclude that although robotic-assisted thoracic surgery is a safe and feasible technique that can achieve the same results as VATS, more studies with a larger number of patients are needed to be able to draw definitive conclusions.7
The only way to determine the validity of this type of robotic approach is to demonstrate similar results in terms of effectiveness and patient safety when compared to thoracoscopy or open surgery. To achieve the above, it is essential to have an adequate volume of patients to allow us to perform the number of procedures required (which may vary from surgeon to surgeon) and to achieve efficiency in their use.
Taking into account the above, the sooner a thoracic surgeon or resident is involved in robotic surgery, the sooner they will reach an acceptable level of competence in practice, which optimizes the results and reduces the incidence of complications.8 In this line, it is important to consider that the number of robotic systems available for teaching in the country is very limited; and even more so, the number of thoracic surgeons certified for their use. It also influences the fact that most of this equipment is still concentrated in private hospitals with limited access for surgeons in training.
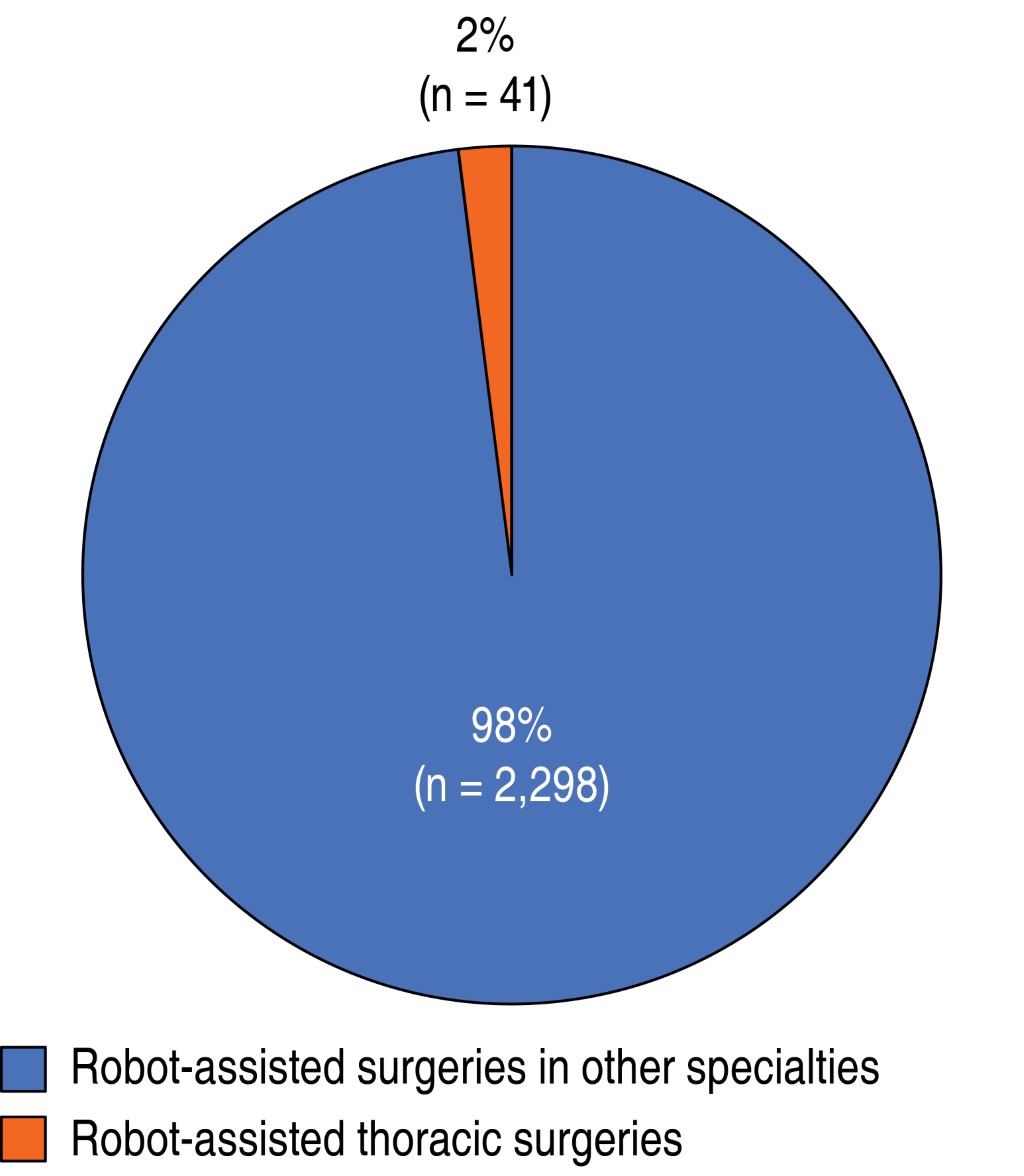
At the Central Military Hospital, robotic surgery program was initiated in 2014, to date a total of 2,339 robot-assisted surgeries have been performed, making it the hospital center that has performed the most procedures of this type in the country (Figure 1). Of the total number of surgeries, 41 correspond to thoracic robotic procedures (Figure 2), of which 20 have been performed in the last year, representing almost 50% of the robot-assisted thoracic surgeries performed. Since the Central Military Hospital is a teaching hospital where the human resources demanded by the army in health care are trained, doctors and surgical residents in training are involved in robotic surgery from early stages, forming a first-hand concept of the advantages, disadvantages and areas of opportunity for the future.
It is also necessary to understand that the success of a robotic surgery program does not only depend on the surgeon; the training of all the personnel involved in the surgical procedure must be considered: anesthesia, nursing, technicians, providers, etc. (Figure 3) and, of course: the institution, which is responsible for the acquisition, maintenance and operation of the equipment. As mentioned above, it is necessary to achieve efficiency in the handling of the robot, which will only be achieved with repeated and constant use.
As surgeons, a large part of our skills should be focused on the aspect of manual dexterity, which will be better the more repetitions of a given procedure are performed. One of the initial disadvantages that have been mentioned in robotic procedures is the absence of the tactile sense, not being in direct contact with the patient and losing the sensation of consistency and texture of the tissues, essential for most of us and which, with practice, should be replaced by a better visualization and localization of the anatomical structures. The more time we use the robotic platform, the more we will become familiar with its use, its capabilities, we will compensate for its disadvantages, we will reduce surgical times, we will reduce costs for a greater number of procedures and, as a consequence, we will favor a better evolution and a faster recovery of the patients.
Our work at a personal level will be to be prepared for the changes, with an open and receptive mind to adopt them in the best way, to change the existing paradigms; exactly the same thing that happened with the introduction of laparoscopic surgery at the end of the 80's; it will be the work of the institution to support and provide the necessary means to offer the best possible treatment, only with this collaboration it will it be possible to materialize a successful program of robotic surgery. The passage of time will be responsible for showing the results; for the time being, we must prepare ourselves and do what we must.
AFILIACIONES
1Hospital Central Militar, Mexico.Conflict of interests: the authors declare that they have no conflict of interests.
REFERENCES