Swyer James MacLeod Syndrome. Case report of hyperlucid lung
Torres-Rodríguez, Servio Tulio1; Reyes-Zúñiga, Karla Marleny1; Chang-Castillo, Iván Estuardo2; Herrera-Cruz, Danilo1
Torres-Rodríguez, Servio Tulio1; Reyes-Zúñiga, Karla Marleny1; Chang-Castillo, Iván Estuardo2; Herrera-Cruz, Danilo1
ABSTRACT
KEYWORDS
James MacLeod Swyer syndrome, hyperlucid lung, case report.Introduction
Swyer James MacLeod syndrome was described simultaneously in 1950 by three professionals, highlighting the interrelation of the different disciplines of medicine, pulmonology and radiology. The three physicians, one of English origin and two Canadians, coincided in the findings of the syndrome that today bears their names. It is related to bronchitis and bronchiolitis obliterans, acquired during childhood from a bacterial or viral infection, and its diagnosis is usually incidental in the course of a radiological evaluation in which unilateral hyperlucency of the lung is revealed.
Clinical case
A 31-year-old female patient consulted a national hospital with a history of mild retrosternal pain, insidious, not radiating and relieved by sleeping. Due to poorly defined findings in the X-ray, chest tomography was requested and she was transferred to our center. She reported a history of respiratory diseases in childhood and adolescence, such as pneumonia, bronchitis, common colds treated as outpatients, and during the pandemic she suffered from uncomplicated COVID-19.
Admitted in good general and nutritional condition, SO2 99%, heart rate (HR) 74 beats per minute (bpm), without dyspnea or cyanosis. Lungs with adequate air entry and rhythmic heart without murmurs. Labs: hemoglobin 13 mg/mL; hematocrit 39%; platelets 224 × 109/L; D-dimer 273.59; alpha 1 antitrypsin 98.8 (82.50-320). Pulmonary function tests: spirometry; FEV1 3.09 (52%) 1.55; FVC 3.64 (59%) 2.13; FEF 25-75% 85.39 (88%) 72.89, suggestive of restriction. Body plethysmography/flow-volume uninterpretable. SB diffusion, DLCO 8.18 (80%) mild decrease. Lenin walk, walks 225 m, being 35% of his predicted, without pauses during the test. NADIR: SO2 88% with no need for supplemental oxygen.
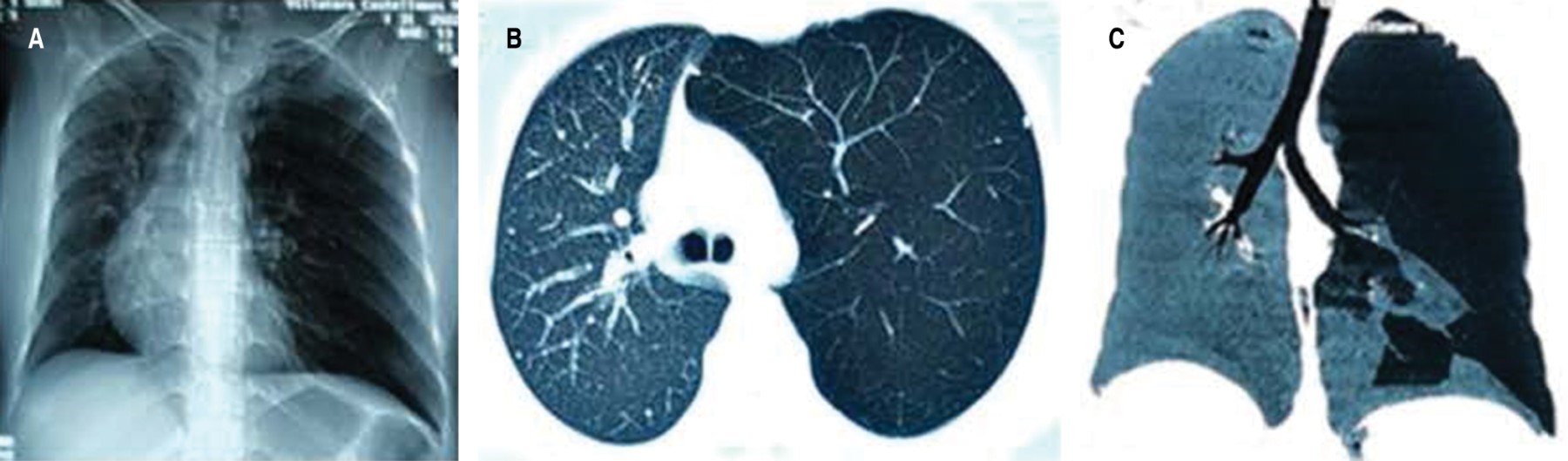
Chest X-ray showed left lung overdistended, displacing the mediastinum to the right and hyperlucent; computed axial tomography (CT) showed, in addition, anomalous distribution of the pulmonary vasculature with areas of hypoperfusion of variable distribution (Figure 1).
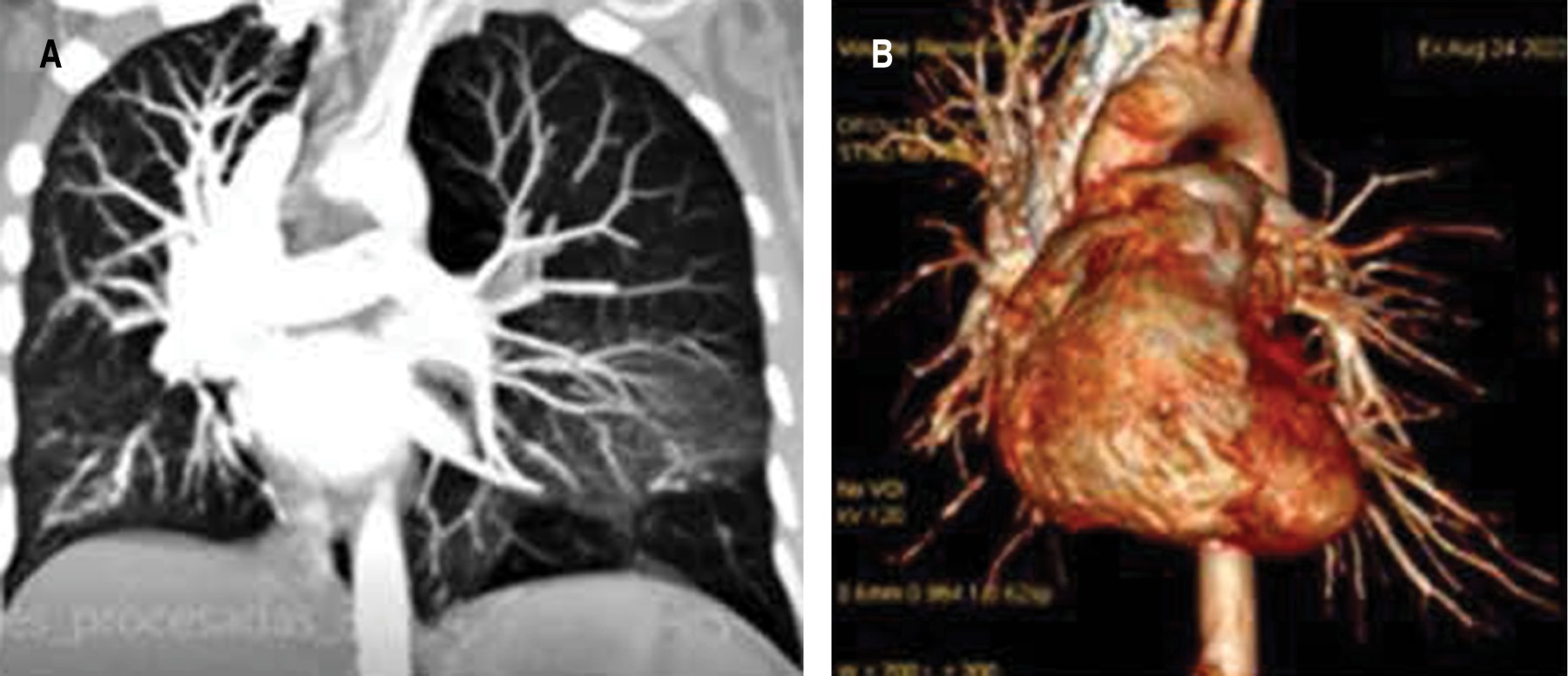
Ruling out probable pulmonary thromboembolism (PTE), CT angiography was requested, which showed no evidence of PTE in the digital reconstructions, showing continuity of opacification of first and second order pulmonary arteries. Lung with left hyperclarity and hypoplasia of the ipsilateral pulmonary artery measuring 9 mm in diameter A-P compared to 20 mm on the right. Consider Swyer James MacLeod syndrome (Figure 2). Echocardiogram, reports dextrocardia with EF at 55%. Low probability of PAH with pulmonary systolic pressure at 20 mmHg. Abdominal CT reports no abnormalities.
Discussion
Swyer James MacLeod syndrome is a rare clinical-radiological entity that reports a prevalence of 0.01% in 17,450 chest radiographs.1,2 We present the case of a young woman with a history of repeated respiratory disorders in childhood, which probably led her to develop structural changes in her lung. Due to the characteristics shown, this syndrome has no defined etiology, but it is related to viral infections such as influenza A virus, respiratory syncytial virus, mumps, paramyxovirus, adenovirus type 3, 7 and 21; as well as a bacterial origin, in which Bordetella pertussis, Mycobacterium tuberculosis and Mycoplasma pneumoniae are involved.1 It is a rare emphysematous disease characterized by obliteration of the small bronchioles, hypoplasia or absence of pulmonary artery and peripheral vascular bed.3 The functional abnormality of this syndrome is undoubtedly diffuse chronic expiratory obstruction with distal air trapping.4 The most distinctive feature compared to emphysema is the absence of chronic obstructive pathology in the small airway,3 which coincides with the FEF 25-75% 85.39 (88%) 72.89 data obtained from the patient.
A mild chest pain prompted consultation and radiography showed a hyperlucent left lung. It is most commonly diagnosed in infancy, typically occurring in children under eight years of age, before the lung has completed lung development and maturation.5 It may run asymptomatically into adulthood, present with usually asymptomatic spontaneous pneumothorax,2 or as a rare emergency condition,3 as calcified bullae6 and with placental transfiguration of the lung parenchyma.7 The patient's chest X-ray and CT scan showed hyperlucent segmental lung with altered vascularity, which is usually described by other authors as unilateral or lobar pulmonary hyperclarity, associated with air trapping of the hyperlucent lung during expiration.2,5,8 In order to rule out the differential diagnosis of pulmonary thromboembolism, angiotomography was requested, which showed anatomical abnormalities of the left pulmonary artery with a smaller caliber and decreased flow. The spirometric pattern showed restrictive process. Pulmonary scintigraphy was not performed that could show decreased ventilation of the pathologic lung secondary to emphysematous changes and a marked decrease in perfusion, as a consequence of the reduced caliber of the pulmonary artery.5,8 Therefore, diagnostic criteria for this syndrome require one of the following findings: a) unilateral loss of lung volume with hyperlucency demonstrated by chest radiography; b) unilateral reduction of vascularity on chest CT scan; and c) unilateral loss of perfusion on technetium-99m lung scan.1,2
Treatment is established according to symptoms and may vary from conservative management to surgical indications. Surgery is reserved for patients with recurrent lung infections that do not respond to conservative treatment or whose symptoms are not adequately controlled with optimal medical treatment. Surgical options include pneumonectomy, volume reduction surgery, lobectomy, or anatomic or non-anatomic segmentectomies,1 performed by thoracotomy, videothoracoscopy or robotics according to preference, experience and availability of resources. Due to their clinically stable evolution, conservative treatment with outpatient follow-up was chosen.
Conclusions
Swyer James MacLeod syndrome is a rare entity that usually presents asymptomatic; its diagnosis is usually an incidental finding and treatment is conservative in most patients, with definite surgical indications.
Acknowledgments
To Dr. Sergio Villeda Castañeda, master in general surgery, and Dr. Elka Lainfiesta Moncada, anesthesiologist, for their contribution to the review of this clinical case.
AFILIACIONES
1Hospital San Vicente, Guatemala, Guatemala 2Clínica Londres, Guatemala, Guatemala.Conflict of interests: the authors declare that they have no conflict of interests.
REFERENCES