Schwannoma, a differential diagnosis in posterior mediastinal tumors
Palomares-Capetillo, Paola1; Armas-Zárate, Francisco Javier1; Iñiguez-García, Marco Antonio1
Palomares-Capetillo, Paola1; Armas-Zárate, Francisco Javier1; Iñiguez-García, Marco Antonio1
ABSTRACT
Tumors of the posterior mediastinum are predominantly neurogenic tumors. Neurogenic tumors arise from tissues whose origin is the embryonic neural crest, and are classified according to whether they grow from the nerve sheath, nerve cells or are paraganglionic. Among the group of benign nerve sheath tumors, schwannomas and neurofibromas are the most common. Schwannoma is the most frequent intrathoracic neurogenic tumor. The cornerstone of treatment of neurogenic tumors, whether benign or malignant, is complete surgical resection, and is important for diagnostic confirmation and to prevent malignant degeneration.KEYWORDS
posterior mediastinum, tumor, schwannoma.Introduction
Mediastinal tumors represent a wide variety of diagnostic possibilities. Tumors of the posterior mediastinum are predominantly neurogenic tumors (53.9%), followed by benign cysts (13.9%) and lymphomas (5%). The incidence of mediastinal neurogenic tumors is 4.1%; they can occur in either compartment; however, 71-95% occur in the posterior mediastinum.1 They typically arise from spinal nerve roots. Most of these tumors occur in adults.2 Malignancy is unusual and they are usually located in the paravertebral sulcus.2
They occur most frequently between the third and sixth decade of life; most are diagnosed incidentally.3 Between 30-40% are asymptomatic at the time of diagnosis. With growth, symptoms occur due to local compression of adjacent tissues and mainly include chest pain, cough, dyspnea, hoarseness, stridor, superior vena cava syndrome and muscle weakness.4
Neurogenic tumors arise from tissues whose origin is the embryonic neural crest; they are classified according to whether they grow from the nerve sheath, from nerve cells, or are paraganglionic.3 Among the group of benign nerve sheath tumors, schwannomas and neurofibromas are the most common, accounting for 90%.4 These are benign, slow-growing lesions that most often arise from spinal nerve roots, but can involve any thoracic nerve.
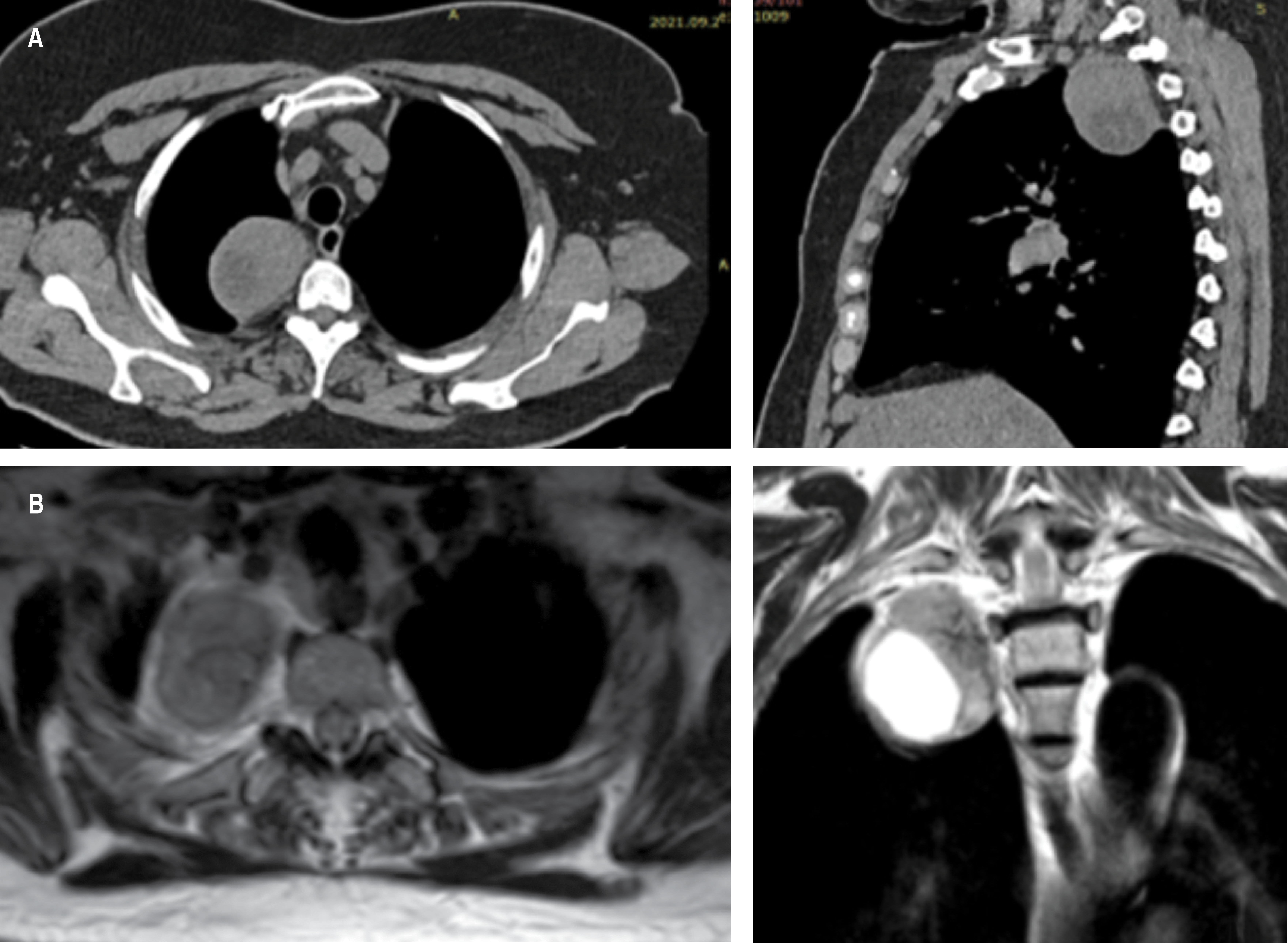
In imaging studies, peripheral sheath tumors are well-defined, hypodense tumors with low attenuation and contrast enhancement on computed tomography (CT). On magnetic resonance imaging (MRI) they are isointense on T1 and hyperintense on T2.1 MRI is the most sensitive method to define the presence and extent of the intraspinal component of the tumor. It is indicated when the tumor is contiguous to the neural foramen, when there is a widened intervertebral foramen, or when there is erosion of a vertebral body or pedicle.5
Schwannoma is the most common intrathoracic neurogenic tumor, accounting for approximately 75% of nerve sheath tumors. It can arise from any neural element within the thorax. They are usually friable and encapsulated. Recurrence and metastases are rare.5-8
Histologically they are composed of Schwann cells, as well as a well-formed capsule. Verocay bodies are another histologic feature, but are neither sensitive nor specific. They are composed of two areas: Antoni A and Antoni B. By immunohistochemistry, they are positive for S100 protein, SOX10, CD57 and GFAP. The cellular variant may have a higher risk of recurrence, but does not show metastatic potential.1,2 Table 1 shows the main differences in the diagnosis of schwannoma and neurofibroma.
The cornerstone of treatment of neurogenic tumors is complete surgical resection, and it is important for diagnostic confirmation and to rule out malignant degeneration.3
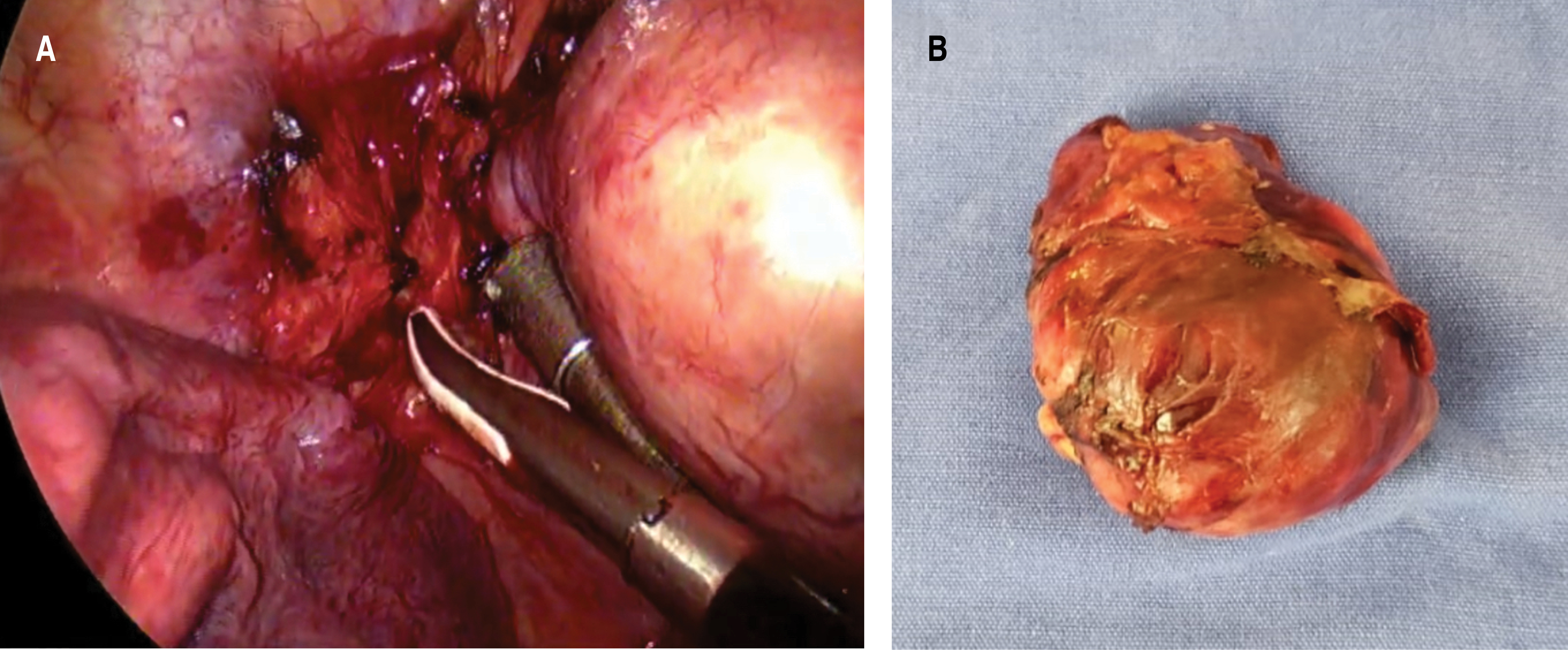
The surgical approach should be decided according to tumor size, location, and intraspinal/neuroforaminal extension or involvement.5 The video-assisted thoracic surgical (VATS) approach is preferred for tumors that show no preoperative signs of malignancy and do not involve the spinal cord.9 As most of these tumors originate from the sympathetic chain, Horner's syndrome is the most feared complication after surgery.3 In more complex cases with an intraspinal component, a combined neurosurgical and thoracic approach incorporating laminectomy followed by thoracotomy or thoracoscopy is usually required to complete the resection.5
Presentation of the case
Female, 67 years old. Important antecedents: allergy to penicillin. Smoking denied. Her condition began after infection by SARS-CoV-2, where a simple chest CT scan was performed with incidental finding of posterior mediastinal tumor (Figure 1A). The study was completed with magnetic resonance imaging (Figure 1B) and the patient was sent to the Thoracic Surgery Service of the Instituto Nacional de Enfermedades Respiratorias Ismael Cosío Villegas, Mexico City. Preoperative examinations and tumor markers were normal. A two-port VATS approach was decided for tumor resection (Figure 2A), with findings of a nerve sheath-dependent tumor at the level of the second intercostal space, whitish, vascularized, 5 × 4 cm in diameter (Figure 2B), which was resected in its entirety without complications. Postoperative evolution was satisfactory, removing the drain on the third day, with adequate lung expansion. Pathology report of a peripheral nerve sheath tumor compatible with schwannoma, with immunohistochemistry positive for PS100 and enolase. Six-month follow-up with no evidence of tumor recurrence.
Discussion
We present a clinical case of a patient with a definitive diagnosis of schwannoma. In our case it was a posterior mediastinal tumor that was an incidental finding in an asymptomatic patient, as in most cases reported in the literature.
In these cases the main differential diagnosis is between schwannoma and neurofibroma, the former being the most frequent in the literature. For the definitive diagnosis, immunohistochemical support is essential to confirm their neurogenic origin and to distinguish between them. In this case, the anatomopathological study showed a neoplasm of mesenchymal origin, encapsulated, with a biphasic growth pattern (Antoni A and Antoni B), mostly myxoid; with nuclear palisade around a fibrillary process (Verocay bodies). Immunohistochemistry was positive for PS100 and enolase, suggesting a diagnosis of schwannoma. In our case, the patient did not meet the criteria for neurofibromatosis, so it was considered a sporadic tumor.10
A minimally invasive approach with two ports was decided based on the size and location of the tumor. This allowed a complete resection and adequate recovery of the patient. Minimally invasive approaches are recommended in the literature depending on the size of the tumor and when there is no suspicion of spinal cord involvement. This allows a shorter hospital stay, less postoperative pain and the same oncologic results.9 However, multiple types of approaches have been described, depending on the characteristics of the tumor and spinal cord involvement.5,9
Complete resection is the cornerstone of treatment. This allows a high cure rate at five years and low recurrence. Long-term follow-up is not well determined, as these are slow-growing tumors, a period of five to ten years is commonly stipulated.
Conclusions
Schwannoma is a differential diagnosis among posterior mediastinal tumors. The studies of choice for diagnosis are computed tomography and magnetic resonance imaging that provide details of the level of tumor involvement. Diagnosis is based on pathology and immunohistochemical features. Treatment is complete surgical resection, ideally by minimally invasive approach, which allows adequate survival and low recurrence.
Acknowledgments
To the Department of Pathology of the National Institute of Respiratory Diseases.
AFILIACIONES
1Instituto Nacional de Enfermedades Respiratorias Ismael Cosío Villegas. Mexico City, Mexico.Conflict of interests: the authors declare that they have no conflict of interests.
REFERENCES
|
Table 1: Histopathologic differences between the main posterior mediastinal tumors. |
||
|
|
Neurofibroma |
Schwannoma |
|
Cytology |
|
|
|
Size of the nucleus |
+ |
++ |
|
Nuclear hyperchromasia |
+ |
++ |
|
Wavy nuclei |
+++ |
+ |
|
Histology |
|
|
|
«Shredded carrot»-type collagen |
+++ |
-/+ |
|
Capsule |
- |
+++ |
|
Hyalinized vessels |
-/+ |
+++ |
|
Fascicular growth pattern |
-/+ |
++ |
|
Mitotic activity |
-/+ |
-/+ |
|
Necrosis |
- |
-/+ |
|
Immunohistochemistry |
|
|
|
S100 |
++/+++ |
+++ |
|
Collagen IV |
++/+++ |
+++ |
|
EMA |
+ |
- |
|
CD34 |
+++ |
+++ |
|
Podoplanin |
+ |
++ |
|
Calretinin |
+ |
+++ |
|
Sox 10 |
+++ |
+++ |
|
EMA = epithelial membrane antigen. |
||


