Repeatability and reproducibility of inspiratory capacity measurement by spirometry and body plethysmography
Vargas-Domínguez, Claudia1; Vázquez-García, Juan Carlos1
Vargas-Domínguez, Claudia1; Vázquez-García, Juan Carlos1
ABSTRACT
KEYWORDS
inspiratory capacity, spirometry, repeatability.Abbreviation:
Introduction
Inspiratory Capacity (IC) is the maximum volume of air that can be inhale continuously from one point to the end of a normal exhalation (tidal volume) to a point of maximum inhalation or total lung capacity (TLC).1,2 The initial point on inhalation of the IC corresponds to the functional residual capacity (FRC), it is a static volume which is also called end expiratory lung volume (EELV). In patients with limited expiratory airflow due to obstructive pulmonary diseases, the EELV is determined by the time constant, tidal volume and the expiratory time.3 Changes in any of these variables that increase the EELV causes an IC decrease. This is functionally relevant because the IC represents a reserve for the tidal volume and, thus, for minute ventilation in exercise conditions.4 IC measuring has been frequently used for investigation purposes; it can be more sensitive than the forced expiratory volume in one second (FEV1) for the quantification of the functional improvement after different therapeutic interventions in patients with chronic obstructive pulmonary disease (COPD). IC predicts dynamic hyperinflation and exercise limitations,5-7 it correlates with syndromes such as dyspnea, bronchodilators response, and exercise tolerance.6,8-17 IC has been use as an improvement indicator in pulmonary rehabilitation programs that involve upper and lower limbs, with or without oxygen therapy18-20 in non-invasive mechanical ventilation21 and in surgery of volume reduction.22 Similarly, IC has been used to define the pulmonary hyperinflation like the relation IC/TLC below 25%. Conceptually, this indicator represents the pulmonary inspiratory fraction and has been described as an important predictor of mortality in patients with COPD.23 IC can be measure by both vital capacity (VC) by body plethysmography. Even when the repeatability and reproducibility of the IC has not been fully explored, the standard of the American and European Societies (ATS/ERS) recommend an IC repeatability of less than 150 mL or less based on the experience of the group and following good practices.2 The objective of this study was to describe the repeatability and reproducibility of the different IC measurement techniques, both by slow spirometry and by body plethysmography in a sample of healthy adults.
Material and methods
A descriptive and prospective study with a convenience sampling was conducted, according to the availability of the laboratory of pulmonary function for the participants studies, who were healthy subjects; most of them workers of the institution, over 18 years of age, without any acute nor chronic respiratory disease history, without respiratory symptoms and without a history of active smoking (less than 400 cigarettes throughout their lives); all of them signed an informed consent form. Subjects who were unable to perform the acceptable maneuvers of forced spirometry, slow spirometry or body plethysmography were removed. Respiratory function tests were always performed in the same order (slow spirometry, forced spirometry and body plethysmography) and as indicated by the ATS/ERS 2005 standards, in force at the time of the study.24 All the tests were performed by expert technicians from the laboratory of pulmonary function and subsequently qualified by the same observer to ensure the criterion of acceptability and repeatability was met. One equipment of respiratory function tests (MasterScreen Body, Jaeger, Hochberg, Germany) was used for all tests. The equipment was calibrated for volume with a three-liter syringe daily before the start of the day. The maximum variability accepted was ± 3%. The subjects were instructed to perform the maneuvers and later a technician demonstrated each maneuver. All subjects performed a forced spirometry, sitting down and in all a minimum of three acceptable maneuvers were obtained, for which up to eight attempts were made. The spirometry must fulfill the repeatability criterion, defined as a difference of less than 150 mL between the two highest values of force vital capacity (FVC) and the two highest values of FEV1.
Inspiratory capacity measurement (IC). Once the subject is seated, the nasal clamp and the mouthpiece of the spirometer were placed, avoiding the presence of air leakage. The individual had to be relaxed and it was requested a normal breathing, for at least three respiratory cycles or until we obtained a stable level of FRC. Two different maneuvers have been described to measure the inspiratory capacity. Maneuver 1 is performed with an IC after reaching a stable level of FRC (no movement of FRC up or down from the level at the end of expiration), the subject should inhale rapidly to the point of TLC (maximum inspiration), followed by a relaxed maximum exhalation until reaching to residual volume (RV). In the maneuver, after obtaining a stable FRC, the subject is asked to exhale completely and in a relax way until a plateau of one second is achieved; after that it is asked to completely inhale until reaching TLC (inspiratory VC) and to exhale completely again in a relaxed way and until reaching a plateau of at least one second (expiratory VC). All subject were able to complete at least three acceptable measurements of VC for both maneuvers with a repeatability less than 150 mL.
Body Plethysmography. The participants were placed inside the cabin sitting straight, and the mouthpiece was adjusted to the appropriate height of the mouth, without bending the neck. The door of the chamber was closed and it was given enough time, usually one minute, for the temperature to equilibrate and the individual to feel comfortable. Afterwards the correct position of the mouthpiece and the nasal clamp was explained; then, it was asked to breath normally (tidal volume) until the FRC was stable, normally between three to 10 breaths. At the end of a normal tidal volume exhalation (FRC level) the obturator occluded, for two to three seconds, and it was requested to performed a series of gentle panting breaths at an approximate frequency of one breath per second. When the obturator reopened, a VC maneuver was completed; equal to the maneuver 1 of slow spirometry. An acceptable maneuver was defined by: 1) stable FRC before occlusion; 2) the difference of volume (DV) at the level of FRC at the time of the valve occlusion should be less than 200 mL; 3)both ends of the plethysmographic FRC curve (FRCpleth) should be visible on the graph; 4) the respiratory rate during the obturation should be approximately 60 breaths per minute (30-90); 5) The FRCpleth curve should be regular and with minimal hysteresis (the inspiration and expiration phases should be practically superimpose); 6) the slope of the measurement line should be parallel to the expiratory part of the FRCpleth curve; and 7) at least, three acceptable FRCpleth maneuvers should be obtain. For the VC maneuver, a plateau of at least one second without change in volume should be reached. Repeatability of the plethysmographic was calculated after obtaining three acceptable maneuvers. The FRCpleth should have a variance of less than 5%. [(higher FRCpleth-lower FRCpleth)/ average FRCpleth]. Moreover, the VC must be repeatable at less than 150 mL between the two of the highest values.
Data Analysis. For the general description of the variables, averages and standard deviation (SD) or, proportions according to the type of variables. The IC variability in mL and in percentage between the two highest values of each test (spirometric and plethysmographic) was quantified as average values in mL and in percent, as well as 90 and 95 percentiles. Additionally, the coefficient of correlation (Pearson r) and graphical concordance analysis was calculated with the Bland et al.25 test for the IC measurements of the spirometry and plethysmography.
Results
A total of 56 participants were included, four subjects who could not perform acceptable forced spirometry maneuvers, two other subjects by IC maneuver 2 and one by plethysmography were eliminated, so the final sample was 49 participants, 27 men and 22 women, with an average age of 33.2 ± 8.3 years (26 to 65 years). Table 1 shows the general, anthropometric characteristics and forced spirometry results of the population studied. Overall, all presented FVC, FEV1 and FEV1/FVC ratio values within baseline limits.
Table 2 shows the repeatability of IC maneuvers performed by slow spirometry and by body plethysmography. The total number of maneuvers performed to obtain a minimum of three acceptable efforts were on average 4.5 ± 1.0 (three to eight efforts) for IC maneuver 1 and 4.5 ± 0.9 (three to eight) for maneuver 2; for plethysmography 5.0 ± 1.1 (three to seven efforts) were performed. In addition, the repeatability values of each test are shown as averages, percentages, and 90 and 95 percentiles (p90, p95). The repeatability of IC was ≤ 150 mL in 96% of participants or ≤ 5% in 98% of subjects for spirometry maneuvers 1 and 2, while for plethysmography it was 78 and 80%, respectively.
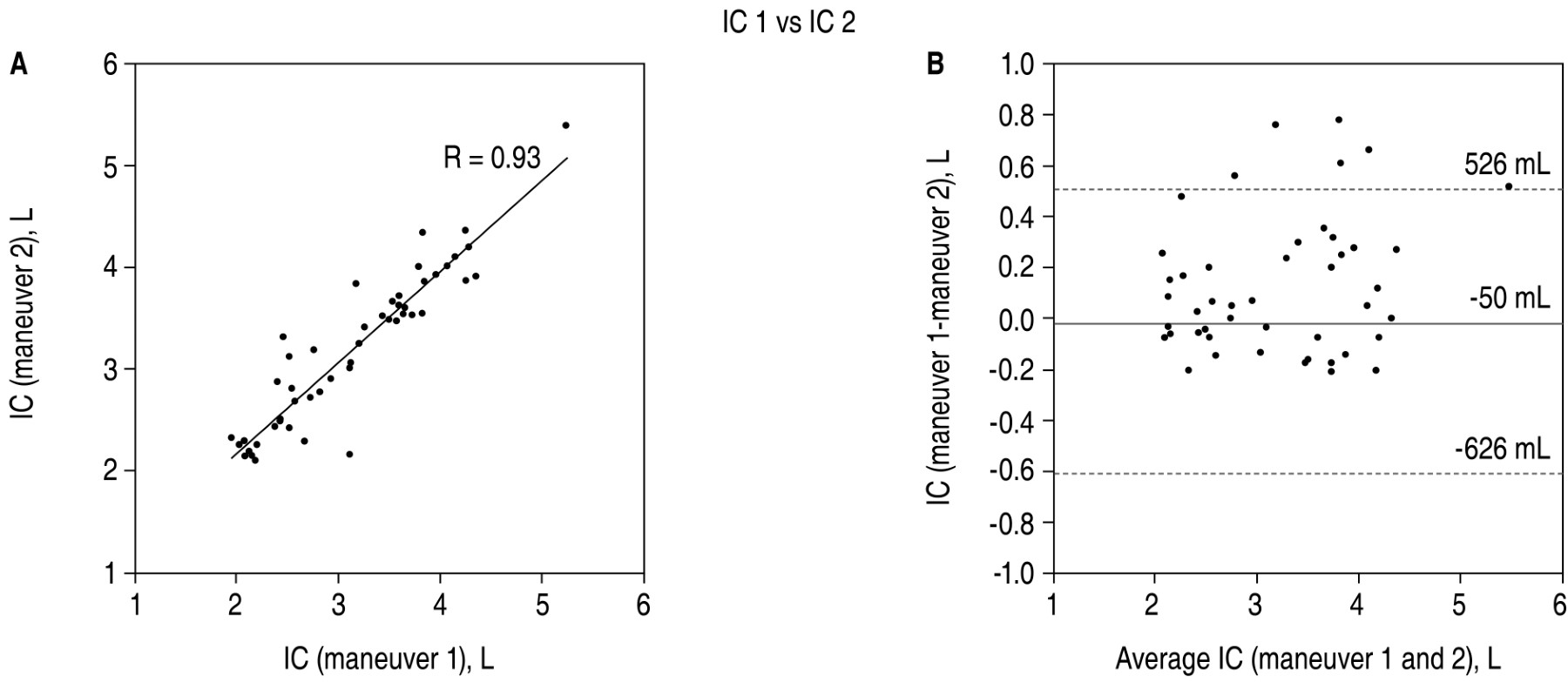
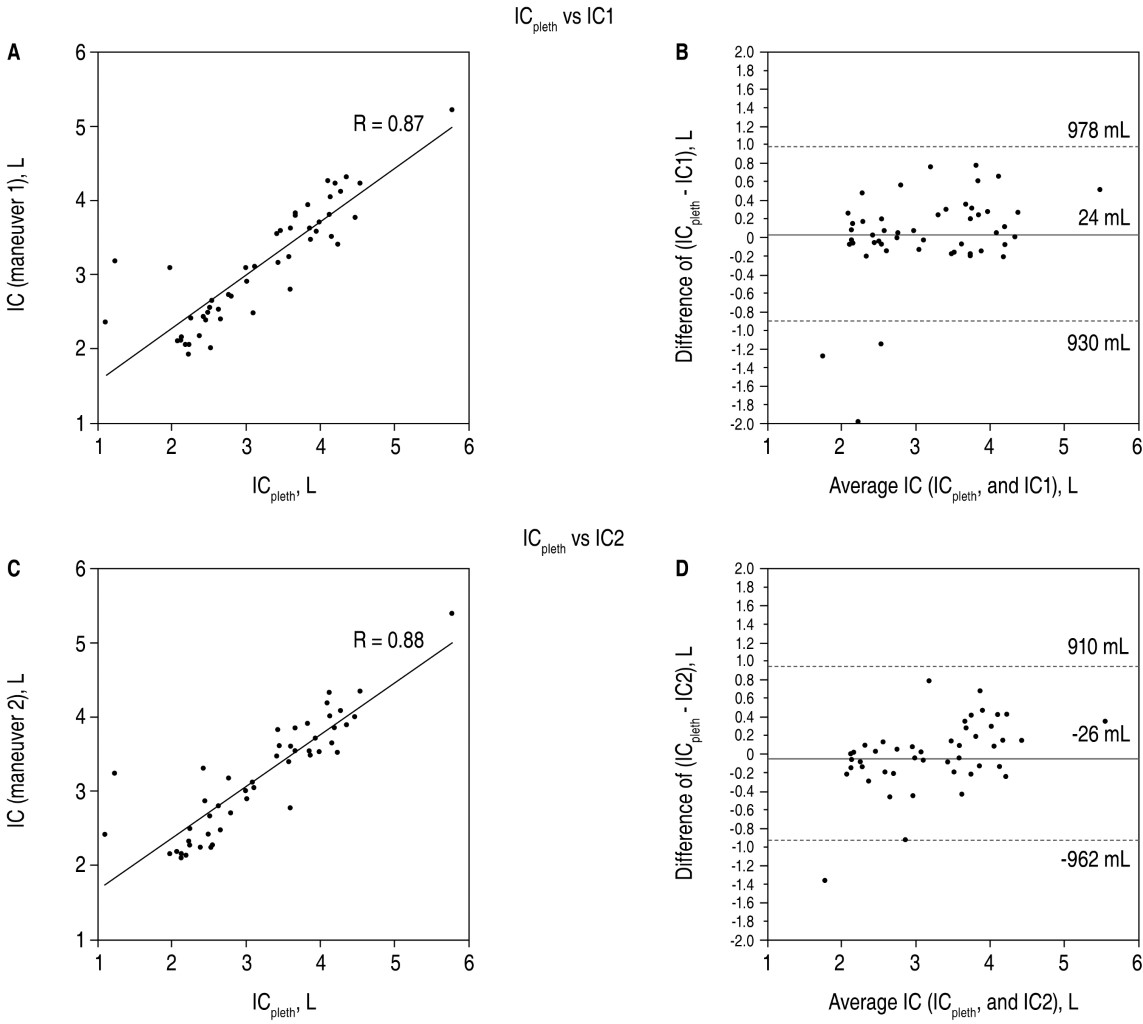
Figures 1 and 2 show the correlation graphs and Bland and Altman graphical analysis of IC between spirometry maneuvers 1 and 2 (Figure 1), as well as maneuvers 1 and 2 versus plethysmography (Figure 2). The CI values with the three measurements were highly correlated (Pearson r) with a correlation coefficient of 0.95 between maneuvers 1 and 2; 0.87 between maneuver 1 and plethysmography, as well as 0.88 between maneuver 2 and plethysmography). However, concordance between measurements (Bland and Altman analysis) showed potential errors of up to 576 mL between maneuvers 1 and 2, 954 mL (maneuver 1 versus plethysmography), and 936 mL (maneuver 2 versus plethysmography.
Discussion
This study explores technical aspects and variability of IC measurement in healthy subjects, both measured by slow spirometry and by body plethysmography. The most relevant results were: 1) the vast majority of subjects were able to perform acceptable maneuvers in all tests; 2) spirometry maneuvers were more repeatable than plethysmography; and 3) in general, all IC measurements had a high correlation; however, in the concordance analysis, potential differences close to a liter are revealed when spirometry is compared with plethysmography.
Initially, the variability of the IC maneuvers obtained by slow spirometry (maneuvers 1 and 2) corresponding to the measurement of IC from FRC (maneuver 1) and measurement of IC subsequent to an inspiratory vital capacity (maneuver 2) was explored, which allowed evaluating the interchange ability of the maneuvers. Both showed similar performance based on the number of maneuvers required to achieve an acceptable test and repeatability values. The criteria for acceptability of IC are those of the slow VC maneuver already described.2 However, the repeatability that can be achieved between maneuvers for IC has not been fully explored. Tantucci et al.26 reported repeatability of 200 mL or less (< 9%) in 241 healthy subjects aged 65 to 85 years. As in any respiratory function test, it depends on the accuracy and precision of the equipment, the required respiratory maneuver, the ability of the technician and the cooperation of the people undergoing the test, as well as their interaction with the technician. Forced spirometry and slow spirometry are known to achieve high repeatability of FEV1, FVC and VC, so repeatability of IC could be expected to be high as well. International spirometry standards ATS/ERS 2019 require repeatability of less than 150 mL for all these values. However, this value is defined based on the experience of the working group and good practices. In this study, for both slow spirometry IC maneuvers, 96% of subjects achieved repeatability of 150 mL or less and in 98% it was ≤ 5%. Consequently, it can be affirmed that any of the spirometric values (FEV1, FVC, VC and IC) are technically very reliable for the purposes of diagnosis, monitoring and measurement of change; as is the case in the bronchodilator response test, in the monitoring of respiratory patients or in people exposed to respiratory risks, as well as in the evaluation of therapeutic interventions.
Another finding of this study is that IC measurements by spirometry achieved better repeatability than plethysmography. The IC measured by plethysmography showed higher repeatability values and with potential differences of almost one liter (Figure 2). This could be explained because the IC maneuver performed by plethysmography is technically more complex and requires greater training and cooperation, as it is done sequentially with the measurement of residual functional capacity (FRCpleth). Plethysmography requires a period in which there is an occlusion of the nozzle obturator (two to three seconds) where the FRCpleth is measured and after that the IC maneuver is performed. In contrast, with slow spirometry, the IC maneuver is performed after a tidal volume expiration. CI values had a good correlation between slow spirometry and plethysmography measurements (Figures 1 and 2). This means that the maneuvers are not completely interchangeable and for follow-up purposes the same test should always be considered, preferably by slow spirometry. The main limitation of this study is that it explores a limited number of healthy subjects and sampling of the studied population was for convenience, which might not be fully representative of the general population or patients with respiratory diseases.
Conclusions
The measurement of IC, mainly when measured by slow spirometry and with any of the accepted maneuvers, showed acceptability and repeatability of 150 mL or less in 96% of the subjects; while for plethysmography it was in 78% of the participants. Overall, all IC measurements had a high correlation coefficient. However, concordance analyses reveal potential differences close to a liter when compared to plethysmographic measurements, so they should not be considered interchangeable. This study supports the current ATS/ERS 2019 spirometry standards recommendation of requiring a repeatability of 150 mL or less for IC measurement.
AFILIACIONES
1Instituto Nacional de Enfermedades Respiratorias Ismael Cosío Villegas. Mexico City, Mexico.Conflict of interests: the authors declare that they have no conflict of interests.
REFERENCES
Graham BL, Steenbruggen I, Miller MR, Barjaktarevic IZ, Cooper BG, Hall GL, et al. Standardization of spirometry 2019 update. An official American Thoracic Society and European Respiratory Society Technical Statement. Am J Respir Crit Care Med. 2019;200(8):e70-e88. Available in: https://doi.org/10.1164/rccm.201908-1590st
Taube C, Lehnigk B, Paasch K, Kirsten DK, Jörres RA, Magnussen H. Factor analysis of changes in dyspnea and lung function parameters after bronchodilatation in chronic obstructive pulmonary disease. Am J Respir Cri Care Med. 2000;162(1):216-220. Available in: https://doi.org/10.1164/ajrccm.162.1.9909054
Marin JM, Carrizo SJ, Gascon M, Sanchez A, Gallego B, Celli BR. Inspiratory capacity, dynamic hyperinflation, breathlessness and exercise performance during the 6 minute walk test in chronic obstructive pulmonary disease. Am J Respir Cri Care Med. 2001;163(6):1395-1399. Available in: https://doi.org/10.1164/ajrccm.163.6.2003172
Casanova C, Cote C, De Torres JP, Aguirre-Jaime A, Marin JM, Pinto-Plata V, et al. Inspiratory to total lung capacity ratio predicts mortality in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2005;171(6):591-597. Available in: https://doi.org/10.1164/rccm.200407-867oc
|
Table 1: General characteristics of the studied population. |
|||
|
Variable |
Men (n = 27) |
Women (n = 22) |
Total (N = 49) |
|
Age, years |
33.7 ± 7.3 (26-51) |
35.1 ± 0.07 (27-65) |
33.2 ± 8.3 (26-65) |
|
Weight, kg |
78.5 ± 10.5 (63-116) |
62.5 ± 9.1 (46-82) |
71.1 ± 12.8 (46-116) |
|
Height, m |
1.75 ± 0.05 (1.64-1.87) |
1.59 ± 0.06 (1.49-1.81) |
1.67 ± 0.10 (1.49-1.82) |
|
BMI, kg/m2 |
25.7 ± 3.1 (21.6-38.3) |
24.6 ± 2.8 (20.0-30.1) |
25.2 ± 3.0 (20-38.3) |
|
*Participants with BMI ≥ 25 kg/m2 |
14 (51.8%) |
10 (45.5%) |
24 (50.0%) |
|
*Participants with BMI ≥ 30 kg/m2 |
1 (3.7%) |
1 (4.5%) |
2 (4.0%) |
|
Forced spirometry maneuver |
4.4 ± 1.3 (3-8) |
4.3 ± 1.5 (3-7) |
4.3 ± 1.3 (3-8) |
|
FVC, L |
5.24 ± 0.65 (3.78-6.54) |
3.55 ± 0.8 (2.66-4.65) |
4.46 ± 1.01 (2.66-6.54) |
|
FVC, %p |
110.0 ± 12.3 (80-139) |
103.9 ± 11.3 (92-128) |
109.3 ± 11.9 (80-144) |
|
FEV1, L |
4.23 ± 0.51 (3.13-5.43) |
2.91 ± 0.43 (2.02-3.98) |
3.62 ± 0.82 (2.02-5.43) |
|
FEV1, %p |
105.1 ± 11.8 (79-144) |
109 ± 11.9 (78-130) |
104.3 ± 11.8 (79-144) |
|
FEV1/FVC, % |
81.8 ± 5.2 (70.7-92.6) |
83.3 ± 5.1 (74.1.6-92.0) |
82.6 ± 5.1 (70.7-92.6) |
|
Values are expressed in mean ± standard deviation (minimum and maximum value), and others in n (%)*. %p = percent predicted. BMI = body mass index. FVC, forced vital capacity. FEV1 = forced expiratory volume in the first second. |
|||
|
Table 2: Repeatability of the inspiratory capacity tests. |
|||
|
Parameter |
Inspiratory Capacity (IC) |
||
|
Maneuver 1 |
Maneuver 2 |
Plethismography |
|
|
Number of maneuvers |
4.5 ± 1.0 (3 to 8) |
4.5 ± 0.9 (3 to 8) |
5.0 ± 1.1 (3 to 7) |
|
Average IC, L |
3.12 ± 0.78 (2.03-5.24) |
3.17 ± 0.74 (2.11-5.32) |
3.15 ± 0.95 (1.09-5.76) |
|
Repeatability in mL Percentile 90, mL Percentile 95, mL
≤ 100 mL, n (%) ≤ 150 mL, n (%) ≤ 200 mL, n (%) |
69.0 ± 68.1 (0-420) 122 150
38 (77.6) 47 (95.9) 48 (98.0) |
72.3 ± 50.2 (0 a 210) 130 146
35 (71.4) 47 (95.9) 48 (98.0) |
108.5 ± 100.0 (0 a 420) 244 318
28 (57.1) 38 (77.6) 41 (83.7) |
|
Repeatability in %
≤ 3 % mL, n (%) ≤ 5 % mL, n (%) ≤ 10 % mL, n (%) |
2.3 ± 2.5 (0-15.3)
22 (44.8) 48 (98.0) 49 (100) |
2.4 ± 1.8 (0-7.4)
20 (40.8) 48 (98.0) 49 (100) |
3.4 ± 3.2 (0-10.8)
30 (61.2) 39 (79.6) 45 (91.8) |
|
Except when otherwise noted, values are expressed in mean ± standard deviation (minimum and maximum value). |
|||


