Airway management in a patient with necrotizing cervical fascitis
Martínez-Sánchez, David Josué1; Waldo-Hernández, Luis Iván1; Palomares-Capetillo, Paola1; Vázquez-Minero, Juan Carlos1
Martínez-Sánchez, David Josué1; Waldo-Hernández, Luis Iván1; Palomares-Capetillo, Paola1; Vázquez-Minero, Juan Carlos1
ABSTRACT
Necrotizing fasciitis is an aggressive skin and soft tissue infection that can rapidly spread through the perifascial planes. It has a high morbidity and mortality and requires aggressive surgical treatment initially to reduce associated morbidity and mortality. The case of a 53-year-old male with a history of diabetes mellitus II who presents a cervical abscess after a tonsillectomy, it evolves to cervical and thoracic fasciitis, drainage of the abscess and open tracheostomy are performed in another hospital. He came to our institute with a dehiscent wound, discharge of purulent material, and air leakage from the tracheostomy site. During the procedure, a 4 cm orifice is identified on the anterior wall of the trachea, debridement and placement of negative pressure therapy is performed. Subsequently, a flap is mobilized over the tracheal orifice, and a Montgomery cannula is placed to close the cervical wound. Control bronchoscopy shows a good tracheal lumen, without stenosis or air leak. It is important in a patient with necrotizing fasciitis to have aggressive surgical treatment initially, taking care of the following principles: adequate drainage of all collections, and debridement of all necrotic tissue and taking care not to contaminate adjacent structures.KEYWORDS
trachea, fasciitis, Montgomery.Introduction
Necrotizing fasciitis is a severe infection of the skin and soft tissues, which causes tissue necrosis and can spread rapidly through the fascial planes.1 The incidence of this infection varies according to reports from different regions, being more frequent in developing countries, the incidence can be up to 1 in 100,000.1 It is usually a polymicrobial infection, which makes adequate antibiotic treatment difficult, in addition to the fact that it spreads rapidly through the tissues. Symptoms are very varied and are related to the affected area and the patient's septic process.
The fundamental pillar of treatment is surgical drainage and debridement, which should always be complemented by adequate resuscitation of the patient and coverage with broad-spectrum antibiotics.2 Cervical infection commonly caused by an odontogenic process carries a high morbidity due to the structures present such as large vessels, digestive tract and airway, in addition to the risk of extension to the mediastinum. Therefore, an adequate initial management, preserving these structures, is fundamental to improve the morbimortality of these patients.3
Case presentation
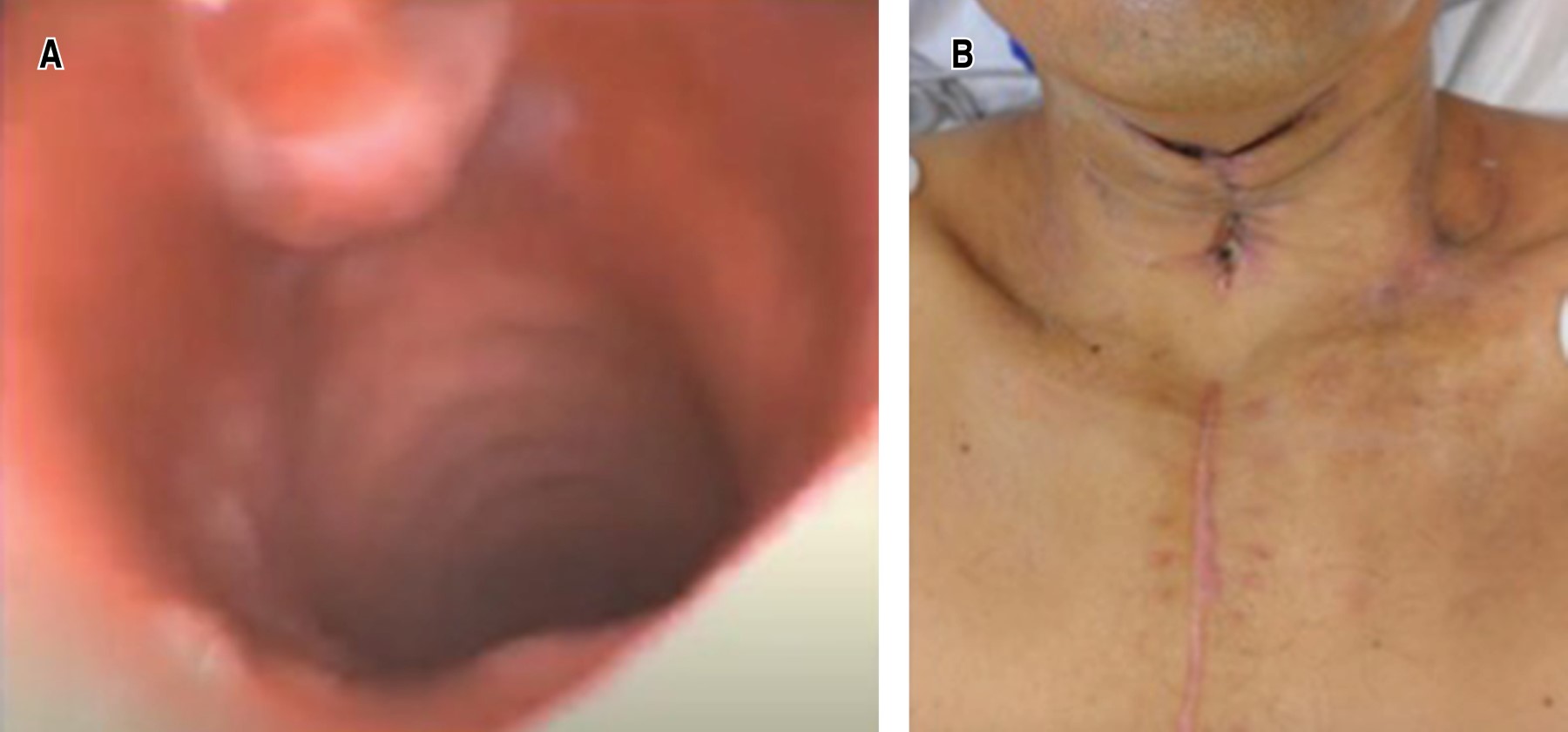
Male, 53 years old, with diabetes mellitus II with treatment, adequate controls and a smoking rate of 12 packs/year. He refers that approximately 10 days before his admission to the Instituto Nacional de Enfermedades Respiratorias Ismael Cosío Villegas, Mexico City, he underwent tonsillectomy which was complicated by a peritonsillar abscess and evolved with cervical and superficial thoracic fasciitis. Abscess drainage was performed with submandibular and cervical approach, placing tracheostomy cannula to ensure airway. She came to our institute presenting wound dehiscence, purulent material leakage, erythema in adjacent tissues and area leakage through the tracheostomy site (Figure 1A).
The wound was debrided and washed, a 4 cm hole was identified in the anterior face of the trachea (Figure 1B) and abundant purulent material. It was decided to replace the tracheostomy cannula and negative pressure therapy (Figure 1C). Subsequently, three reexchanges were performed, partially closing the wounds. To ensure and achieve closure of the trachea while maintaining an adequate lumen, it was decided to place Montgomery cannula and mobilize on the same sternocleidomastoid flap, achieving total closure of the wound. Then, on an ambulatory basis, the patient was decannulated and revision bronchoscopy was performed, observing an adequate tracheal lumen, with no evidence of fistula or air leak (Figure 2).
Discussion
Necrotizing fasciitis, as previously mentioned, presents high morbimortality and is associated with a large number of complications. Treatment should be timely and aggressive, taking into account the following points: broad-spectrum antibiotic therapy, aggressive surgical debridement in the first 24 hours, adequate airway management and constant re-evaluation of the patient.3
In the past, it was believed that performing a tracheostomy in patients with significant cervical infection was the ideal management to secure the airway and adequately ventilate patients; however, this procedure increases morbidity and presents long-term complications. The infectious process could more easily spread to the mediastinum and poor tracheostomy cannula placement can lead to long-term stenosis.4 Today, with the development and availability of technology, video laryngoscopy or bronchoscopy can be used to assist in intubation and preserve tracheal integrity.
Many times, due to the extent of the infectious process and tissue necrosis, extensive debridement is necessary, resulting in large defects of the skin and underlying tissues. Multiple articles have compared in-hospital stay, number of re-interventions and wound evolution using simple cures versus negative pressure therapy, favoring the latter.5 Therefore, its use is recommended to improve tissue healing and allow early wound closure.
Likewise, when there is a large lesion or defect in the airway, either secondary to an infectious process or as a complication of a procedure, it is important to be able to reconstruct and maintain its integrity to ensure adequate ventilation and improve patient morbidity. In this case it was decided to use a Montgomery cannula, which is normally used for tracheal stenosis not candidates for surgical treatment; nevertheless, due to its characteristics, it allowed to ensure the patient's ventilation and phonation, as well as to provide adequate support to mobilize a flap and allow granulation and closure.6,7
Conclusions
It is important to timely diagnose a soft tissue infection in the cervical region and to offer adequate treatment from the first intervention. This will give the patient the best opportunity to reduce the number of re-interventions, reduce the morbidity associated with the condition and the procedure, and facilitate the resolution of the septic process. In the absence of the equipment or expertise to manage these cases, it is important to consult or refer to the appropriate service or institution. As stated in the literature, and in this case, the use of negative pressure therapy is essential for the treatment of these wounds, the integrity of the trachea should be preserved whenever possible.8 Providing timely comprehensive management and using all available resources can reduce the morbidity and mortality associated with this condition.7,9,10
AFILIACIONES
1Instituto Nacional de Enfermedades Respiratorias Ismael Cosío Villegas. Mexico City, Mexico.Conflict of interests: the authors declare that they have no conflict of interests.
REFERENCES