Extragonadal mixed germ cell tumor primary of the mediastinum. Case report
Sánchez-Zazueta, Eduardo1; Miyagui-Adame, Kiyoshi Alejandro1; Gamez-Sainz, Ilse Lorenia1; Galaviz-Humo, Jesús1
Sánchez-Zazueta, Eduardo1; Miyagui-Adame, Kiyoshi Alejandro1; Gamez-Sainz, Ilse Lorenia1; Galaviz-Humo, Jesús1
ABSTRACT
Germ cell tumors are usually neoplastic located in the testicles or ovaries manifested in early life. Extragonadal germ cell tumors are infrequent, representing 1 to 3% of extragonadal germ cell neoplasms. When they present, they are usually 1 to 2 excisions, the anterior mediastinum representing the most common site. They are usually asymptomatic in 20-40% of patients until there is compression or obstruction of nearby structures and there are no symptoms. We present the case of a 22 year old male without comorbidities who started with cough without hourly predominance, hemoptysis, fever, unintentional weight loss, diaphoresis, orthopnea, physical examination revealed pleuropulmonary condensation syndrome, cabinet studies were performed. initially chest X-ray confirmed by tomography chest, abdomen, pelvis, testicular ultrasound and serum studies a mass in the mediastinum located in the anterior compartment, a biopsy was taken and removal of the mediastinal mass, concluding in a primary extragonadal tumor of mixed germ cells of the mediastinum composed of three cell excisions, representing a diagnostic challenge due to their large size. were re offered treatment with chemotherapy based on bleomycin, etoposide, and cisplatin in four cycles without new relapses.KEYWORDS
mixed germ cell tumor, alpha-fetoprotein, mediastinum.Introduction
Primary mediastinal germ cell tumors are rare neoplasms, which have been found to be due to malignant transformation of germ cells that migrate during embryogenesis. In these tumors there is an alteration of the epiblast in its migration and descent, leading to the formation of a late mediastinal tumor.1,2
They are divided into two groups: seminomatous and nonseminomatous germinal tumors. Seminomas represent 30%, while nonseminomatous represent 70%, subdivided into mature teratomas with 44%, immature teratomas 6%, yolk sac tumors 60%, tumors derived from primitive embryonic cells, representing embryonal carcinoma 5%, tumors of extraembryonic differentiation such as choriocarcinoma 2%.1,2
The germinal locations described as extragonadal at the level of the mediastinum are rare, representing 1 to 3% of the extragonadal germinal neoplasms, 1.27 cases per 1'000,000 inhabitants are found without evidence of a primary testicular tumor; another location is the retroperitoneum.3-5
At the time of diagnosis, 20-40% of patients are asymptomatic. The initial diagnostic methods are testicular ultrasound to rule out primary gonadal origin, followed by tomographic extension study including chest, abdomen and pelvis. Tumor markers such as alpha-fetoprotein and human gonadotropin are not diagnostic alone, but are useful to guide prognosis. Biopsy is the diagnostic study of choice; when performing it, immunohistochemistry with markers such as OCT4, SALL4 should be requested to confirm the origin of cells as they have high sensitivity for primary mediastinal seminomas and embryonal carcinomas; in cases where the histological diagnosis is not conclusive, karyotyping can be performed in order to identify p12 isochromosomes, which is a cytogenetic anomaly of tumors with germ lineage.
Current recommended treatments of choice are chemotherapy followed by resection of the residual mass. Chemotherapy schedules are similar to those used in tumors of testicular origin with cisplatin-based chemotherapy achieving long-term complete remissions in 50% of cases. The most commonly employed chemotherapeutic scheme includes three to four cycles of cisplatin in combination with etoposide and bleomycin. If after completion of chemotherapy treatment, imaging tests reveal persistence of residual masses, optimal resection of these is usually indicated; up to 30% of primary mediastinal germ cell tumors may show tumor remnants, and suboptimal resection is useful in these cases. When relapse or refractoriness to initial treatment occurs, current salvage chemotherapy regimens are based on paclitaxel or ifosfamide in combination with cisplatin.6,7
Due to the infrequency of extragonadal disease we consider this report relevant, even more so because it is a young patient and a mixed germinal tumor in a greater proportion of endodermal sinus; there are very few cases described in the literature, those reported are usually teratomas and the mixed mediastinal variety.
Clinical case
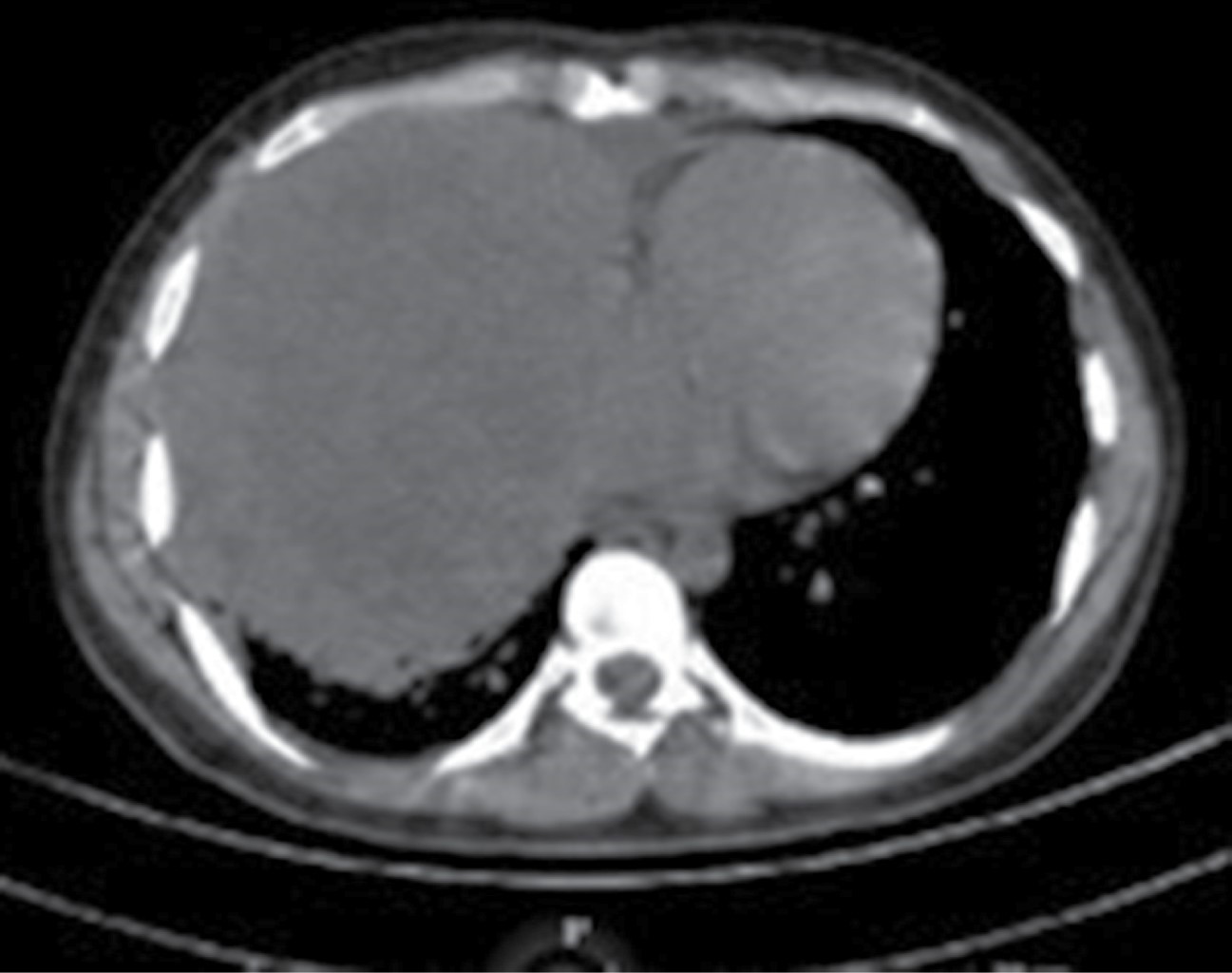
22-year-old male with no chronic degenerative history. He started with a non-cyanotic, non-emitting cough. After two months of evolution he went to the doctor where viral infection was suspected; two weeks later he persisted with cough accompanied by hemoptysis, orthopnea, nocturnal diaphoresis, weight loss of 7 kg in three months, fever of 39°C. When the symptoms did not improve, a chest X-ray was performed, finding incidentally a mediastinal mass. Subsequently, tomography of the chest, abdomen and pelvis revealed an anterior mediastinal tumor measuring 14 × 13 cm in the right hemithorax, with displacement of mediastinal structures towards the left hemithorax. Because of age and form of presentation, lymphoma was suspected (Figure 1A). Physical examination was compatible with a pleuropulmonary condensation syndrome; a 5 mm right inguinal adenopathy, indurated and immobile, was also found. Labs were requested, highlighting grade 2 anemia, platelets 622,000/mm3, lactate dehydrogenase 645 u/L, leukocytes 9,000/mm3, glucose 92 g/dL, creatine 0.9 mg/dL, albumin 3.9 g/dL, negative viral panel, tumor markers with result alpha-fetoprotein 3,080 ng/mL, carcinoembryonic antigen 0.98 ng/mL, human chorionic gonadotropin hormone 0.78 ng/mL. Testicular ultrasound showed a simple cyst in the head of the left epididymis of 1 mm. During his hospitalization, he underwent mediastinal biopsy for cardiothoracic surgery in conjunction with resection of tumor mass by thoracotomy; during the trans-surgical event he presented massive hemorrhage of 4,000 milliliters with hypovolemic shock grade 4 requiring massive transfusion; resection in fragments of mediastinal mass was achieved (Figure 1B). Post-surgical findings, mediastinal mass of 12 × 10 cm with fragments larger than 1 cm in the thorax because they were adhered to the pulmonary hilum and, representing a greater risk of bleeding, merited placement of a 36 fr right pleural tube. After the suboptimal tumor resection procedure, the cough, orthopnea, hemoptysis and thermal elevations subsided; the patient was discharged after a good clinical evolution (Figure 2). The biopsy findings were compatible with mixed germinal tumor of the endodermal sinus type 70%, seminoma 25%, embryonal carcinoma 5% with extensive tumor necrosis of 50% of the surgical specimen (Figure 3). Immunohistochemistry showed diffuse positive SALL 4, negative OCT3/4, focal positive AFP, focal positive D2-40 (1%), focal positive PLAP (5%), negative CEA-CD30. He was evaluated by the medical oncology service, which granted chemotherapy with bleomycin, etoposide, cisplatin in four cycles; and also follow-up by the pulmonology, cardiothoracic surgery, medical oncology services where, after five months of post-surgical evolution and with control chest CT scan, the patient remains asymptomatic, with follow-up by multidisciplinary outpatient clinic due to risk of compression of surrounding structures and new relapse.
Discussion
Extragonadal germ cell tumors usually debut with chest pain, cough, dyspnea, hemoptysis, fever. Our patient started with this symptomatology to which unintentional weight loss was added; a mediastinal mass was observed on chest X-ray, which is the initial study as part of the approach in patients who debut with cough of unknown etiology and is useful to rule out differential diagnoses, mainly infectious. As part of the protocol, a tomography of extension to the thorax, abdomen and pelvis was performed, which confirmed mediastinal mass; tumor markers were requested for predictive purposes, alpha-fetoprotein elevation suggestive of nonseminomatous tumor was found; suspecting a primary gonadal origin, testicular physical examination and testicular ultrasound were performed to rule out the presence of tumor in this site; a cyst in the epididymis was found in the patient. Due to the absence of tumor in the gonads and the previous tomographic findings in the mediastinum, he was evaluated by the Cardiothoracic Surgery area. He requested a mediastinal biopsy as part of the diagnostic protocol being the gold standard; the result showed a mixed variety germinal tumor composed of endodermal sinus, seminoma, embryonal carcinoma. The next step was immunohistochemistry for confirmation purposes; the immunohistochemistry was compatible with SALL 4, AFP, D2-40, PLAP positive.
The first-line treatment for nonseminomatous germ cell tumors is chemotherapy followed by surgical resection. Currently, the drug of choice for chemotherapy is cisplatin, which achieves complete remission in 50% of cases. The preferred scheme of choice includes three to four cycles of cisplatin at a dose of 20 mg/m2 combined with etoposide 100 mg/m2/day for five days and bleomycin 15 mg/m2 weekly. Once these cycles have been completed, monitoring should be carried out with a cabinet study; if the residual mass persists, surgical resection is indicated; when the residual tumor is larger than 1 cm, suboptimal resection is chosen, and when there is no macroscopic residual tumor, optimal resection is considered. During the biopsy, due to the size of the tumor and the parahilar location, suboptimal surgical resection of the tumor mass was performed with subsequent chemotherapy based on bleomycin, etoposide and cisplatin in four cycles, which must be individualized for each patient. After achieving tumor remission with chemotherapy, all patients should be followed up, since up to 50% usually relapse in the first two years. When relapse or refractoriness to treatment occurs, the rescue chemotherapy regimens are paclitaxel 135 to 250 mg/m2/day every three weeks or ifosfamide 1,200 mg/m2/day for five days plus cisplatin, monitoring hematologic and nephrologic toxicities. The patient, currently, after five months of evolution, remains asymptomatic after treatment with monthly follow-up, due to the risk of mediastinal mass overgrowth and compression of structures due to the poor prognosis as it is a germinal tumor of three cell lines.4-10
Conclusion
Extragonadal germinal tumors debut clinically when the disease is advanced due to compression of neighboring structures, so an early histopathologic diagnosis is essential. During the biopsy of the patient, a suboptimal tumor resection had to be performed in the same surgical time, due to the large size and parahilarity of the tumor, with the risk of bleeding. As these tumors were vascularized, the patient had a drainage of 4,000 milliliters, so he had to undergo transfusion and endopleural catheterization; subsequently he had a good evolution. The histopathological result was a mediastinal tumor of mixed germinal variety not previously described in the literature. Treatment must be individualized, being essential to focus on the subtype of germinal tumor; preoperative chemotherapy makes the mediastinal tissues fibrotic and worsens surgical planning, so in this patient tumor resection followed by chemotherapy was of greater benefit.
AFILIACIONES
1Instituto Mexicano del Seguro Social, Unidad Médica de Alta Especialidad Hospital de Especialidades No. 2 Luis Donaldo Colosio Murrieta. Centro Médico Nacional del Noroeste. Obregon City, Sonora, Mexico.Conflict of interests: the authors declare that they have no conflict of interests.
REFERENCES