Effect of a physical exercise and education program in patients with diffuse interstitial lung diseases
Betancourt-Peña, Jhonatan1,2; Rivera, Julian Andrés1,3
Betancourt-Peña, Jhonatan1,2; Rivera, Julian Andrés1,3
ABSTRACT
KEYWORDS
lung diseases interstitial, dyspnea, quality of life, exercise tolerance, idiopathic pulmonary fibrosis.Introduction
Diffuse interstitial lung disease (DILD) represents a set of conditions that involve the alveolar and capillary basement membranes, i.e., the anatomical interstitium;1 more than 150 different types of DILD are currently known, however, it is only possible to establish the etiological diagnosis in approximately 30-40% of cases.1
These diseases have been classified as having similar clinical features (dyspnea as the predominant symptom), radiological (diffuse pulmonary infiltrates), physiological (preferential alteration of gas exchange), and anatomopathological (preferential alteration of lung support tissues).2 However, the most commonly reported type of DILD is idiopathic pulmonary fibrosis (IPF).1
In terms of incidence and prevalence, it differs substantially given the methodology used to diagnose it, in turn, changes in the classification and appearance of new entities make it difficult to collect epidemiological data; these diseases occupy one of the first places of morbidity and mortality in the world. In the United Kingdom the prevalence is 1.5 to 1.8 per 10,000 inhabitants, while in Spain there was an incidence of 7.6 per 100,000 inhabitants.3
There are environmental or exogenous factors that are involved in the pathogenesis of the disease, not to mention also endogenous factors such as gastroesophageal reflux and autoimmunity,3 among the sociodemographic risk factors found in the appearance of DILD are considered male, be over 40 years of age and have been an active smoker for more than 30 packs in the year.4
As for the diagnosis of DILD, the clinical evaluation includes factors such as exercise intolerance, limitation in ventilation, gas exchange, diffusion and circulation, which deteriorate the individual early, in addition to functional capacity and health-related quality of life.3 Some diagnostic aids, such as chest radiography , allow observing alterations of interstitial predominance with patterns: reticulonodular, ground glass and honeycomb.5 In addition to this diagnostic aid, currently high-resolution computed axial tomography (CAT) has shown sensitivity in terms of the diagnosis of DILD.5 Restrictive alteration is generally evident in spirometry, with a decreased forced vital capacity (FVC) in relation to the forced expired volume in the first second/normal forced vital capacity (FEV1/FVC) and the reduction of the diffusion capacity of carbon monoxide (DLCO) turns out to be a frequent finding.1 Functional tests, such as the six-minute walk test (6MWT), turn out to be a predictor of mortality and help to individually assess patients.6
Exercise intolerance is one of the most frequent conditions in patients with DILD, it is usually related to the sensation of dyspnea during exertion and progressive increase in fatigue, which causes a worse quality of life.7 Changes in respiratory pattern and decreased tidal volume further functionally limit patients with DILD, so pulmonary rehabilitation is widely recommended since clinical improvements have been documented in 6MWT, dyspnea and health-related quality of life (HRQoL).8
However, there are few studies in our context that report interventions related to pulmonary rehabilitation (PR) in subgroups of patients with DILD, since the behavior may not be the same. For this reason, the objective of this study was to establish the effects of PR in patients with IPF and other DILD on dyspnea, functional capacity, anxiety/depression, and HRQoL.
Material and methods
A quasi-experimental study in which all patients with DILD who met the inclusion criteria were linked for convenience and completed a physical exercise and education program in a clinic in the city of Cali, Colombia, during 2019.
This study took into consideration and adopted the recommendations of the declaration of Helsinki and was approved by the Ethics Committee of the participating Institution according to minutes 126.01.05.02, which classified it as research with a risk greater than the minimum according to resolution 008430 of 1993 of the Ministry of Social Protection of Colombia.
Patients who met the following inclusion criteria were linked: diagnosis of DILD through a medical history confirmed by a radiologist and pulmonologist and in those cases that merited additional examinations, they were diagnosed by a multidisciplinary medical team through chest X-rays, pulmonary function tests and CAT, for which two groups were formed (IPF and other DILD),9,10 admission to the physical exercise and education program of the clinic for the first time, so that at the time of admission they had not received exercise recommendations and all participants were sedentary/inactive. Exclusion criteria were patients with beta-blocking or anti arrhythmic drugs, presence of pacemakers, cardiac arrhythmias, uncontrolled arterial hypertension (160/100 mmHg), saturation during 6MWT < 80% and other uncontrolled cardio metabolic diseases and presenting respiratory comorbidity such as chronic obstructive pulmonary disease (COPD) and asthma.
For the development of the study, the following variables were taken into account: age, sex, place of residence, socioeconomic status, type of DILD, post bronchodilator volume flow curve spirometry FEV1, FVC, FEV1/FVC taken from the patients' medical records. At the beginning and end of the physical exercise and education program, the variables were taken: dyspnea in the activities of daily living of the Medical Research Council (MRC), peripheral oxygen saturation (SpO2), weight, body mass index (BMI), for functional aerobic capacity the distance traveled in the 6MWT, anxiety/depression with the Hospital Anxiety and Depression Scale (HADS) questionnaire and HRQoL with the Saint George's Respiratory Questionnaire (SGRQ).
Measurements
In a first encounter, 6MWT was performed in the morning in a 30-meter-long corridor, in which the patient was instructed to walk as fast as possible for 6 minutes in a path delimited by two cones.11 SpO2 and heart rate were measured through a pulse oximeter (NONIN GO2 FINGER pulse oximeter® PN# 9570). At the end of the TC6M, the distance traveled in meters and the VO2e (estimated oxygen consumption) were obtained with the formula VO2e = 3.5 mL/kg/min + (vel m/min × 0.1).12
After the 6MWT, the HADS hospital anxiety and depression questionnaire was applied to each of the participants; this questionnaire takes into account the score obtained for each subscale with values of 0-3, the score range being between 0-21, it is considered normal when the anxiety or depression subscale has a score of 0-7, doubtful of 8-10 and clinical problem greater than 11.1,13
At the end, the SGRQ questionnaire was carried out in a self-directed manner, which includes 50 questions that are distributed in the domains symptoms, activity and impact; the score obtained varies between 0 = best performance and 100= worst performance.1
Physical exercise and education program
The physical exercise and education program was carried out for 24 sessions, carrying out three sessions per week for eight weeks of exercise and educational activities. The patients performed continuous exercise in recumbent bicycle and endless band for 30 minutes starting at 50% of the VO2e obtained in the 6MWT that increased to 80%, supplementary oxygen was administered to those patients who presented a desaturation in the 6MWT ≥ 4% or who during the exercise the SpO2 was < 90%.1,14 Muscle strengthening of the upper limbs was performed with four sets of 12 repetitions with a minute of rest at 40% of the maximum resistance (MR), which increased to 60% of the MR at four weeks; the progression of the exercise was carried out taking into account the score in the modified Borg dyspnea always maintaining the activities between 3-5/10. In education activities, patients received individual and group sessions on the following topics including: disease awareness, medication optimization, oxygen use, feeding, panic measures, relaxation techniques, and home breathing exercises.14 Patients were also educated and encouraged to increase their levels of physical activity beyond the program on non-training days.14
Statistical methods
The information collected was entered in a Microsoft Office Excel® 2010 book in which a database was built that was then analyzed in the SPSS statistical package version 24; through descriptive tests the qualitative variables were presented in frequency and percentage, through the Kolmogorov-Smirnov test the parametric behavior of the quantitative variables was assumed presenting them in mean ± standard deviation; to compare the variables at the beginning and end after the physical exercise and education program in the groups, a t test was performed for paired samples; in turn, the results were compared between the IPF group and the group of other DILD at the beginning and end of the physical exercise and education program by performing the t test for independent samples. A significance of 95% and a p-value < 0.05 was considered statistically significant.
Results
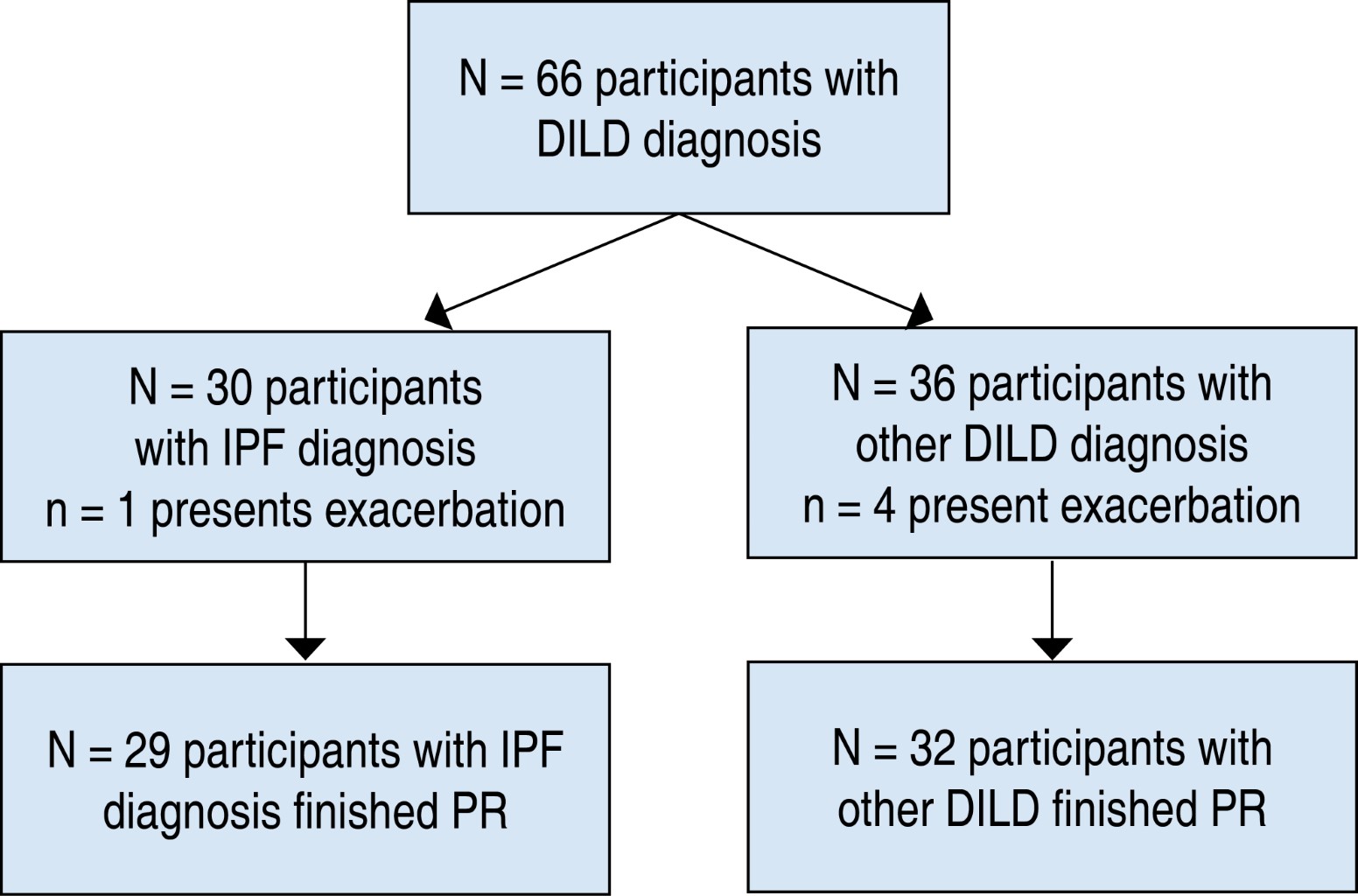
66 patients were initially linked to the study, 30 with IPF and 36 with other DILD; however, during the rehabilitation sessions one patient with IPF and four patients with other DILD presented exacerbation so they left the PR program (Figure 1).
The majority of participants were found to be male, 55.7%; age showed a mean of 61.05 ± 16.24 years. Regarding the socioeconomic stratum, it was found that the highest percentage was classified as medium with 79.3% in IPF and 50.0% in DILD followed by classified as low and finally high. Compared to the type of interstitial disease, 29 patients equivalent to 100% belonged to the IPF group, followed by other unclassified DILD 56.3%; pneumoconiosis 18.8%; interstitial pneumonitis 12.5%; silicosis 6.3% and lupus 6.3% respectively; finally, lung function shows reduced forced vital capacity (FVC) in both groups (Table 1).
Regarding the changes in the 6MWT pre- and post-program of exercise and education, it is found in the IPF group statistically significant improvement going from 371.79 ± 121.39 meters to 435.38 ± 109.75 and clinically with an increase of 63.59 ± 12.67 meters; the same happens in the DILD group where a statistically significant improvement is shown going from 353.0 ± 121.13 meters to 415.0 ± 107.91 meters and clinically significant of 62.00 ± 8.19 meters. The functional aerobic capacity shows that the estimated VO2 shows a statistically significant improvement in the IPF group from 9.47 ± 2.16 mL/kg/min pre PR to 10.77 ± 1.82 mL/kg/min post PR; the same response is evident in the DILD group from 9.17 ± 2.12 mL/kg/min to 10.43 ± 1.79 mL/kg/min post PR. In addition, six patients with IPF (20.1%) and five with other DILD (15.6%) required the use of supplemental oxygen during 6MWT, a situation that required these patients to perform it during exercise sessions. Dyspnea measured with the MRC scale shows a statistically significant change when comparing pre- and post- PR data in both the IPF and DILD groups; the same is true for the HADS scale for anxiety and depression in both groups (Tables 2 and 3).
The health-related quality of life, measured with the SGRQ questionnaire in the IPF group and DILD group shows statistically and clinically significant changes in the domains of symptoms, activity and impact with a pre PR total score in the IPF group of 50.14 ± 18.90 points and post PR of 34.00 ± 17.40 points with a difference of 16.14 ± 2.22 points; the same results are evidenced in the DILD group where a pre PR total score of 54.78 ± 17.58 points and post PR of 44.53 ± 19.11 points with a difference of 10.25 ± 3.04 points is presented (Tables 2 and 3).
When comparing the results obtained from the means versus pre- and post-exercise tolerance PR between the two groups IPF and DILD, a statistically significant change was evident only at the end of the intervention in the HADS questionnaire for depression with a value of p = 0.047 (Table 4).
Discussion
The objective of this study was to establish the effects of a physical exercise and education program in patients with IPF and other DILD on dyspnea, functional aerobic capacity, anxiety/depression and health-related quality of life, for which it was important to understand that IPF and DILD comprise a great heterogeneity and individual variety due to their pathological process, where we can find different causal factors and benefits of exercise according to the type of DILD.
Taking into account the above, this study found that the male sex occurs more frequently in other DILDs, which may be due to a greater relationship with a decrease in steroid hormones such as dehydroepiandrosterone responsible for decreasing fibroblast proliferation and increasing apoptosis.15 However, it contrasts with other authors who show prevalences in men of 72.4% in patients with IPF.16
With respect to age, this study shows that participants have an average age of 61.05 ± 16.24; despite understanding that IPF and DILD can have genetic compromises and be generated at any stage of life, it has been found that their symptomatology hasa greater presentation from adulthood where, being more predisposed to these diseases, some authors mention that some components of RNA telomerase promote fibrogenesis,15 in the same way it is related to what was described by other authors in the context of rehabilitation programs.16
In both IPF and DILD, a decrease in the percentage of the predicted FVC was found through spirometry, evidencing a possible restrictive ventilatory pattern with greater compromise in the group of other DILDs, which was classified as moderately severe and moderate in the IPF group, which is due to the fact that in these two diseases an important restrictive compromise is generated due to their pathological process related to inflammation and attempts at tissue repair, which leads to loss of elasticity of the pulmonary parenchyma, thus decreasing pulmonary ventilation and gas exchange, producing hypoxia and subsequently dyspnea as an initial symptomatology in patients.17
There were no significant changes in BMI in the comparison groups; this could be due to the time of intervention in the physical exercise and education program, since they are not long enough to generate changes that contribute to the decrease of the fat component in this type of patients.18,19 In addition, this study did not carry out a nutritional control and follow-up that will cause relevant changes related to the intervention.
It was found that the IPF group travels a greater distance in the 6MWT than the DILD group, but this difference is not significant; it is evident that both groups significantly improve the distance traveled in the 6MWT due possibly to the fact that physical exercise performed in this type of patients contributes to improving oxygen transport and oxygen exchange at the tissue level, which contributes to greater fatigue resistance due to better beta-oxidation and oxidative phosphorylation at the mitochondrial level, which contributes to the generation of energy in the muscle fiber and as a result a better tolerance to exercise also expressed in better functional aerobic capacity.16 It was found that the IPF group travels a greater distance in the 6MWT than the DILD group, but this difference is not significant; it is evident that both groups significantly improve the distance traveled in the 6MWT due possibly to the fact that physical exercise performed in this type of patients contributes to improving oxygen transport and oxygen exchange at the tissue level, which contributes to greater fatigue resistance due to better beta-oxidation and oxidative phosphorylation at the mitochondrial level, which contributes to the generation of energy in the muscle fiber and as a result a better tolerance to exercise also expressed in better functional aerobic capacity.16
The SpO2 in the two groups IPF and DILD show significant desaturation during 6MWT, which is due to a decrease in alveolar ventilation and gas exchange due to the restrictive ventilation pattern generated in their pulmonary parenchyma, which does not change after the exercise and education program and even these two diseases do not show significant differences when evaluating SpO2 after 6MWT.7 It is important to note that this situation described above forced 11 patients of all of them to use supplemental oxygen during the exercise sessions; however, this situation showed that there were no differences between the intervention groups, so both groups had similar functional performance conditions, both in 6MWT and in the exercise sessions.7,20
In the dyspnea measured with the MRC scale, it was evidenced that both groups of patients presented a significant improvement; a situation that can be explained because the exercises performed in the exercise and education program allows the training of peripheral muscles causing a better tolerance to the effort evidenced in the increase of the distance traveled in the 6MWT.16
For both groups of patients , there was a significant improvement in anxiety after the physical exercise and education program, this could occur since the patients presented improvements in MRC dyspnea related to effort tolerance and activities of daily living, a situation that allows patients to improve their capacity and functional independence.21,22 Additionally, the group of patients with IPF presented significant improvements in the depression domain of the HADS questionnaire, this related to the greater increase in this group of patients in the distance traveled in the P and the lower MRC dyspnea score that allows patients to perceive greater functional independence and less care by caregivers.23
Changes in HRQoL show that patients with IPF and other DILDs improve clinically and significantly in the domains of symptoms, activities and impact; however, the IPF group shows greater changes in SGRQ scores compared to the group of other DILDs. These results are related to the benefits reported by other authors;24,25 additionally, patients with IPF usually have a worse clinical prognosis, which clearly shows that they benefit more from a structured exercise program and educational sessions that allow them to better perceive their disease in relation to the environment around them.26
This study is relevant since interventions related to exercise and education in patients with DILD have not been well documented in Latin America. In turn, this study could be a benchmark in future studies that decide to implement similar interventions to benefit patients in variables such as functional aerobic capacity, dyspnea, anxiety/depression and HRQoL.
The main study limitations are related to the pulmonary function tests used in patients, given that plethysmography and DLCO provide more relevant information on the structural deterioration and prognosis of patients. On the other hand, being one of the first studies in our context that differentiates the effects of exercise and education according to the type of DILD, the implementation of other strategies such as respiratory muscle strengthening, intermittent and interval exercise could show additional gains to those already reported in this study. In addition, it can be considered a possible bias to consider that the exercise was only carried out in the context of the program and that the patients did not exercise in the context of the home or their social relationships. On the other hand, aspects related to pharmacological treatment with steroids, or an analysis by subgroup of patients with supplemental oxygen use during exercise sessions, were not taken into account in this study, which can clearly influence the final result of the measurements. Finally, the quasi-experimental design of this study considerably affects the external validity of the study, so randomized controlled clinical trial designs are recommended in future investigations.
Conclusions
Patients with IPF and other DILDs who undergo an eight-week exercise and education program at a clinic in Cali, Colombia, have a similar increase in distance traveled on the 6MWT, significant improvements in functional aerobic capacity, dyspnea in activities of daily living CRM, and anxiety in all health-related quality of life domains. Depression only showed significant improvement in the IPF group.
Acknowledgements
To patients who voluntarily participated in the study.
AFILIACIONES
1Institución Universitaria Escuela Nacional del Deporte. Cali, Colombia 2Escuela de Rehabilitación Humana, Universidad del Valle. Cali, Colombia 3Universidad Libre. Cali, Colombia.Conflict of interests: the authors declare that they have no conflict of interests.
REFERENCES
Travis WD, Costabel U, Hansell DM, King Jr TE, Lynch DA, Nicholson AG, et al. An official American Thoracic Society/European Respiratory Society statement: update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med. 2013;188:733-748. doi: 10.1164/rccm.201308-1483ST.
Yamamoto-Furusho JK, Sarmiento-Aguilar A, García-Alanis M, Gómez-García LE, Toledo-Mauriño J, Olivares-Guzmán L, et al. Hospital Anxiety and Depression scale (HADS): validation in Mexican patients with inflammatory bowel disease. Gastroenterol Hepatol. 2018;41(8):477-482. doi: 10.1016/j.gastrohep.2018.05.009.
He GX, Li N, Ren L, Shen HH, Liao N, Wen JJ, et al. Benefits of different intensities of pulmonary rehabilitation for patients with moderate-to-severe COPD according to the GOLD stage: a prospective, multicenter, single-blinded, randomized, controlled trial. Int J Chron Obstruct Pulmon Dis. 2019;14:2291-2304. doi: 10.2147/copd.s214836.
Betancourt-Peña J, Rodríguez-Castro J, Rosero-Carvajal HE. Oxigenoterapia domiciliaria y capacidad aeróbica en pacientes con enfermedad pulmonar intersticial difusa. Estudio transversal. Rev Cuba Investig Biomed [Internet]. 2022;41:e1263. Disponible en: http://scielo.sld.cu/pdf/ibi/v41/1561-3011-ibi-41-e1263.pdf
|
Table 1: Socio-demographic and clinical characteristics. |
||||
|
Variables |
Total N = 61 n (%) |
IPF N = 29 n (%) |
DILD N = 32 n (%) |
p |
|
Sex Male Female |
34 (55.7) 27 (44.3) |
14 (48.3) 15 (51.7) |
20 (62.5) 12 (37.5) |
0.390
|
|
Age (years)* |
61.05 ± 16.24 |
64.97 ± 16.09 |
57.50 ± 15.78 |
0.072 |
|
Socioeconomic status Low Medium High |
16 (26.2) 39 (63.9) 6 (9.8) |
4 (13.8) 23 (79.3) 2 (6.9) |
12 (37.5) 16 (50.0) 4 (12.5) |
0.070
|
|
Place of residence Cali Outside of Cali |
58 (95.1) 3 (4.9) |
29 (100.0) 0 (0) |
29 (90.6) 3 (9.4) |
0.272 |
|
Type of interstitial disease Idiopathic pulmonary fibrosis Lupus erythematosus Pneumoconiosis Silicosis Interstitial pneumonia Other unclassified DILDs |
29 (47.5) 2 (3.3) 6 (9.8) 2 (3.3) 4 (6.6) 18 (29.5) |
29 (100.0) 0 (0) 0 (0) 0 (0) 0 (0) 0 (0) |
0 (0) 2 (6.3) 6 (18.8) 2 (6.3) 4 (12.5) 18 (56.3) |
NA
|
|
FEV1* (% predicted) |
63.72 ± 17.65 |
68.57 ± 18.36 |
59.33 ± 16.02 |
0.040 |
|
FVC* (% predicted) |
60.06 ± 13.52 |
63.44 ± 13.38 |
56.99 ± 13.10 |
0.062 |
|
FEV1/FVC* (%) |
90.62 ± 21.23 |
89.16 ± 19.51 |
91.94 ± 22.90 |
0.613 |
|
IPF = idiopathic pulmonary fibrosis. DILD = diffuse interstitial lung disease. FEV1 = forced expired volume in the first second. FVC = forced vital capacity. * Values expressed in mean ± standard deviation. |
||||
|
Table 2: Changes in anthropometrics, functional aerobic capacity, dyspnea anxiety/depression and health-related quality of life in patients with IPF (N = 29). |
||||
|
Variables |
IPF, mean ± SD |
p |
||
|
Physical exercise and education |
Mean differences ± SE |
|||
|
Initial |
Final |
|||
|
Weight (kg) |
67.03 ± 13.24 |
67.41 ± 13.78 |
-0.37 ± 0.49 |
0.434 |
|
BMI (kg/m2) |
26.23 ± 4.47 |
26.36 ± 4.6 |
-0.13 ± 0.17 |
0.459 |
|
Distance travelled 6MWT (m) |
371.79 ± 121.39 |
435.38 ± 109.75 |
-63.59 ± 12.67 |
0.000 |
|
SpO2 at rest (%) |
95.90 ± 2.70 |
95.62 ± 2.61 |
-0.28 ± 0.37 |
0.463 |
|
SpO2 final (%) |
88.86 ± 8.85 |
89.10 ± 5.70 |
0.24 ± 0.74 |
0.747 |
|
Desaturation percentage |
7.03 ± 4.99 |
6.52 ± 5.03 |
-0.51 ± 0.68 |
0.452 |
|
VO2e (mL/kg/min) |
9.47 ± 2.16 |
10.77 ± 1.82 |
-1.31 ± 0.29 |
0.000 |
|
MRC |
2.10 ± 1.01 |
1.10 ± 1.08 |
1.0 ± 0.15 |
0.000 |
|
HAD anxiety |
6.31 ± 5.11 |
3.83 ± 3.37 |
2.48 ± 0.65 |
0.001 |
|
HAD depression |
5.52 ± 4.09 |
3.83 ± 2.98 |
1.69 ± 0.59 |
0.008 |
|
SGRQ symptoms |
50.90 ± 20.23 |
36.00 ± 17.68 |
14.90 ± 3.06 |
0.000 |
|
SGRQ activities |
61.83 ± 20.99 |
48.41 ± 28.99 |
13.41 ± 4.61 |
0.007 |
|
SGRQ impact |
40.86 ± 22.18 |
24.41 ± 16.77 |
16.45 ± 2.59 |
0.000 |
|
SGRQ total |
50.14 ± 18.90 |
34.00 ± 17.40 |
16.14 ± 2.22 |
0.000 |
|
IPF = idiopathic pulmonary fibrosis. SD = standard deviation. SE = standard error. BMI = body mass index. 6MWT = 6 minute walk test. SpO2 = partial oxygen saturation. VO2e = estimated oxygen consumption. MRC = Medical Research Council. HAD = hospital anxiety and depression scale. SGRQ = Saint George’s respiratory questionnaire. |
||||
|
Table 3: Changes in anthropometrics, functional aerobic capacity, dyspnea anxiety/depression and health-related quality of life in patients with other DILDs (N = 32). |
||||
|
Variables |
Other DILDs, mean ± SD |
p |
||
|
Physical exercise and education |
Mean differences ± SE |
|||
|
Initial |
Final |
|||
|
Weight (kg) |
67.84 ± 14.26 |
68.66 ± 13.72 |
-0.82 ± 0.48 |
0.098 |
|
BMI (kg/m2) |
31.16 ± 5.34 |
31.46 ± 5.32 |
-0.29 ± 0.17 |
0.102 |
|
Distance travelled 6MWT (m) |
353.0 ± 121.13 |
415.0 ± 107.91 |
-62.00 ± 8.19 |
0.000 |
|
SpO2 at rest (%) |
95.22 ± 2.72 |
95.31 ± 2.73 |
-0.09 ± 0.69 |
0.893 |
|
SpO2 final (%) |
86.94 ± 6.8 |
86.91 ± 5.59 |
0.031 ± 0.88 |
0.972 |
|
Desaturation percentage |
8.28 ± 5.93 |
8.38 ± 5.24 |
-0.09 ± 0.79 |
0.906 |
|
VO2e (mL/kg/min) |
9.17 ± 2.12 |
10.43 ± 1.79 |
-1.26 ± 0.23 |
0.000 |
|
MRC |
2.38 ± 1.07 |
1.78 ± 1.26 |
0.59 ± 0.21 |
0.007 |
|
HAD anxiety |
5.38 ± 3.79 |
3.81 ± 3.33 |
1.56 ± 0.46 |
0.002 |
|
HAD depression |
5.25 ± 3.52 |
4.34 ± 4.41 |
0.91 ± 0.69 |
0.198 |
|
SGRQ symptoms |
51.97 ± 18.38 |
38.28 ± 17.40 |
13.69 ± 3.12 |
0.000 |
|
SGRQ activities |
68.31 ± 18.30 |
57.25 ± 22.67 |
11.06 ± 3.24 |
0.002 |
|
SGRQ impact |
44.59 ± 19.79 |
35.84 ± 20.26 |
8.75 ± 3.81 |
0.029 |
|
SGRQ total |
54.78 ± 17.58 |
44.53 ± 19.11 |
10.25 ± 3.04 |
0.002 |
|
DILD = diffuse interstitial lung disease. SD = standard deviation. SE = standard error. BMI = body mass index. 6MWT = 6 minute walk test. SpO2 = partial oxygen saturation. VO2e = estimated oxygen consumption. MRC = medical research council. HAD = hospital anxiety and depression scale. SGRQ = Saint George’s respiratory questionnaire. |
||||
|
Table 4: Comparison of changes in anthropometric variables, functional aerobic capacity, dyspnea anxiety/depression and health-related quality of life. |
||||
|
Variables |
Physical exercise and education |
|||
|
Initial Mean differences ± SE |
p |
Final Mean differences ± SE |
p |
|
|
Weight (kg) |
-0.81 ± 3.5 |
0.819 |
1.24 ± 3.5 |
0.726 |
|
BMI (kg/m2) |
4.93 ± 5.67 |
0.328 |
5.09 ± 5.7 |
0.351 |
|
Distance travelled 6MWT (m) |
-18.79 ± 31.09 |
0.548 |
0.47 ± 27.89 |
0.468 |
|
SpO2 at rest (%) |
-0.68 ± 0.69 |
0.334 |
0.66 ± 0.69 |
0.655 |
|
SpO2 final (%) |
-1.93 ± 1.63 |
0.243 |
0.13 ± 1.45 |
0.134 |
|
Desaturation percentage |
1.25 ± 1.41 |
0.381 |
0.16 ± 1.32 |
0.164 |
|
VO2e (mL/kg/min) |
-0.30 ± 0.55 |
0.590 |
-0.34 ± 0.46 |
0.472 |
|
MRC |
0.27 ± 0.27 |
0.314 |
0.68 ± 0.30 |
0.424 |
|
HAD anxiety |
-0.94 ± 1.14 |
0.417 |
-0.02 ± 0.86 |
0.648 |
|
HAD depression |
-0.27 ± 0.97 |
0.785 |
0.52 ± 0.97 |
0.047 |
|
SGRQ symptoms |
1.07 ± 4.94 |
0.829 |
2.28 ± 4.57 |
0.915 |
|
SGRQ activities |
6.49 ± 5.03 |
0.206 |
8.84 ± 6.63 |
0.127 |
|
SGRQ impact |
3.73 ± 5.40 |
0.490 |
11.43 ± 4.68 |
0.429 |
|
SGRQ total |
4.64 ± 4.67 |
0.324 |
10.53 ± 4.68 |
0.851 |
|
SE = standard error. BMI = body mass index. SpO2 = partial oxygen saturation. VO2e = estimated oxygen consumption. MRC = medical research council. HAD = hospital anxiety and depression scale. SGRQ = Saint George’s respiratory questionnaire. |
||||


