Complicated pleural effusion in Kartagener syndrome: clinical case presentation
Carbajal-Zárate, Mary Carmen1; Sandoval-Contreras, José Gerardo1; Rodríguez-Amaro, Shanik Aracely1; Armilla-Rivera, Luis Ángel1
Carbajal-Zárate, Mary Carmen1; Sandoval-Contreras, José Gerardo1; Rodríguez-Amaro, Shanik Aracely1; Armilla-Rivera, Luis Ángel1
ABSTRACT
The Kartagener triad; chronic sinusitis, bronchiectasis and situs inversus totalis occur in the syndrome of the same name, with a prevalence of one in every 20 to 40 thousand individuals. This syndrome corresponds to one of the causes of primary pulmonary dyskinesia in adults (unlike the majority present since childhood). These patients have the characteristic of suffering from repeated community-acquired pneumonia, consequence of alterations in ciliary movement to be able to eliminate mucus and the presence of chronic sinusitis that generates purulent secretion, which will move until it reaches the alveoli, reason that complicates the prognosis in this type of patients. We present a clinical case of a 40-year-old male patient with complicated pleural effusion secondary to repeated respiratory infections, as a consequence of primary pulmonary dyskinesia. This is a case of a rare disease since the complete triad characteristic of Kartagener's syndrome can be of extraordinary presentation.KEYWORDS
Kartagener, dyskinesia, bronchiectasis, pleural effusion, infection.Introduction
Kartagener syndrome is the cause of 50% of primary ciliary dyskinesias (PCD), as well as generating bronchiectasis in adult patients, mainly young.1 It has an average age of presentation of 23 years of age, even though there are reported cases of adolescent patients and even up to the fifth decade of life.2 The triad of Kartagener occurs in only one in every 20 to 40 thousand individuals with ciliary dyskinesia; it is characterized by the presence of chronic sinusitis that is almost always diagnosed in childhood. The situs inversus totalis is mostly incidental, since it usually does not generate clinical symptoms, however, a small proportion of patients can develop congenital heart diseases; bronchiectasis develops in adulthood as a result of repeated respiratory infections.3 The classic clinic corresponds to recurrent respiratory infections that, if not adequately treated, can lead to complications such as severe pneumonia, complicated pleural effusion and even total lung transplants due to damage secondary to bronchiectasis.4 In addition, patients experience infertility in 100% of cases, because the cilia of the reproductive systems are defective and do not confer adequate mobility to sperm in men, or adequate adherence of the ovary to the fallopian tubes women.5
Case presentation
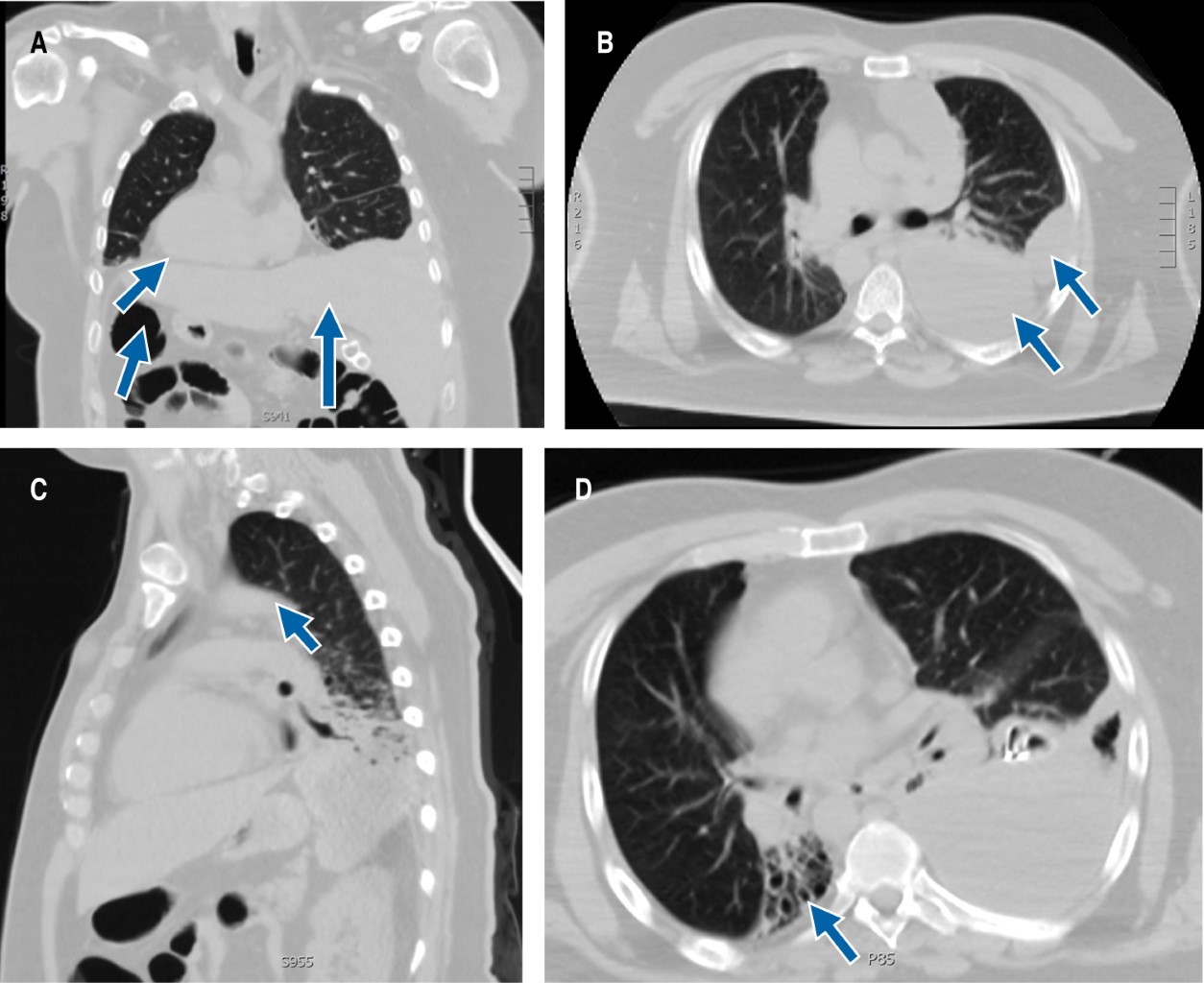
Male patient of 40 years of age, married, without children, with a history of essential arterial hypertension of six-month diagnose in treatment with ARA-II (angiotensin II receptor antagonists), adequate control. History of chronic sinusitis of 31 years of diagnosis without treatment; carrier of situs inversus totalis is reported at nine years of age. Recurrent hospitalization secondary to community-acquired pneumonia, that until now had not conditioned any complication. He began suffering from unquantified fever, shortness of breath and cough, therefore, he is admitted to the emergency area. Laboratory studies were carried out that reported slight leukocytosis at the expense of neutrophilia, increase in acute phase reactant (PCR 50.04), the rest of the paraclinical studies in reference values according to the laboratory. The chest X-ray (not available) showed desxtrocardia, atelectasis, and area of condensation at the base of the right hemithorax; it does not respect the anatomical plane, so it is considered an atypical image. Rapid test is performed for SARS-CoV-2 that is negative. A contrasted computerized axial tomography (CAT) of the chest and abdomen is requested with a report of situs inversus totalis (Figure 1A), mass in the left based and in the anterior mediastinum (Figure 1B and 1C), with slight contrast enhancement, in addition to bibasal bronchiectasis (Figure 1D). Based on laboratory and imaging results, treatment is provided for community-acquired pneumonia (CAP), pneumonia severity index (PSI) of 70 points risk class III, with dual antibiotic treatment. Because the clinic, mainly the cough, did not yield a sputum culture was carried out, with a seven-day growth of Granulicatella elegans; a treatment scheme established by a decrease of 50% the initial PCR value is maintained. Complete course of complicated pleural effusion at the expense of loculations; endopleural probe was placed to try to drain effusion without any success, without obtaining a sample for cytological and cytochemical shipments of pleural fluid. He was moved to the chest surgery area for decortication due to complicated pleural effusion, of probable parapneumonic origin due to repeated infections, secondary to pulmonary dyskinesia with inadequate removal of the ciliary mucus that conditions encapsulation.
Discussion
Primary pulmonary dyskinesia corresponds to a genetic defect with autosomal recessive inheritance linked to the X chromosome, involving genes 4 and 12; since there is a defect in the embryonic nodal cilia, they determine the situs inversus totalis, since the location of the organs during embryogenesis depends on them. Kartagener syndrome is characterized by the triad of situs inversus totalis, bronchiectasis and chronic sinusitis; in addition, it is common to find infertility problems in adult patients due to lack of ciliary mobility in sperm.5
Clinically, it is characterized by the presence of recurrent upper respiratory infections that depend on the presence of chronic purulent sinusitis, and lower by the lack of mobility of the cilia that are the main determinants of the formation of bronchiectasis; this has allowed the development and research of new pulmonary physiotherapy techniques as part of the preventive approach.6 In recent years, genetic techniques have been studied, which would reduce future complications by starting preventive treatment early. Treatment consists of treating the complications with pulmonary physiotherapy, pneumococcal and influenza vaccination. Antibiotic prophylaxis with azithromycin has been proposed for 6 to 12 months in individuals with recurrent complications, but there is still insufficient scientific evidence, despite the fact that it has been proven that morbidity and mortality have significantly decreased in the patients in whom it has been used.4 Among the surgical options, lobectomy and lung transplantation stand out, which has been used successfully in patients with major complications that are life-threatening; the disadvantage is that highly specialized national health centers are required to perform them.3 The preventive approach is the main objective in Kartagener syndrome; if all patients will have the possibility of performing ciliary video microscopy with ciliary sampling or genetic testing, prophylactic measures could be implemented early, and in this way avoid complications in the future.4
Conclusions
Kartagener syndrome corresponds to the main cause of pulmonary dyskinesias; the main complication corresponds to the course of recurrent respiratory infections.
The main therapeutic approach in the future should be prevention, as well as offering new early detection techniques to all patients detected with upper respiratory tract infection and situs inversus totalis or partial.
AFILIACIONES
1Hospital General de Zona No. 1, Instituto Mexicano del Seguro Social. San Luis Potosí, México.Conflict of interests: the authors declare that they have no conflict of interests.
REFERENCES