Pulmonary and endobronchial mucormycosis: a case report
Rabadan-Armenta, Saúl Javier1; García-Torres, María Elena1; Hernández-Hernández, Mario Abel1
Rabadan-Armenta, Saúl Javier1; García-Torres, María Elena1; Hernández-Hernández, Mario Abel1
ABSTRACT
The case of a male patient who was admitted to the pulmonology department for a diagnostic protocol for left apical cavitation is presented. One of the risk factors he had was type 2 diabetes. His condition began with productive cough, whitish sputum, and dyspnea. During the diagnostic process, a bronchoscopy study was performed, revealing endobronchial invasion. Samples were taken, and in the initial assessment, tuberculosis was ruled out due to its high prevalence in our region. Ultimately, the diagnosis was established as pulmonary mucormycosis and an uncommon endobronchial mucormycosis, both of which have a high mortality rate.KEYWORDS
pulmonary mucormycosis, amphotericin B, air-crescent sign, mucormycosis endobronchial.Introduction
Mucormycosis is an opportunistic infection caused by mucoral fungi of the class Zygomycetes.1 These mucoral fungi are ubiquitous, saprophytic and not very demanding; they are found in soil or decaying organic matter. Among them, three genera are known to be pathogenic to humans: Rhizopus, Absidia and Mucor. Their optimum growth temperature is 28 to 30 °C under aerobic conditions, with an incubation period of two to five days. Incubation may begin with inhalation of spores or direct inoculation of injured skin.2 The most common types of mucorales isolated from patients with mucormycosis are Absidia, Rhizopus and Rhizomucor. These species are believed to be ubiquitous saprophytes and soil is their main habitat. Sporangiospores released by the mucorales range in diameter from 3 to 11 µm and can aerosolise, which disperses them into the environment and can lead to upper or lower respiratory tract infections.2
Pulmonary mucormycosis is the third most common presentation of this disease and is characterised by its aggressive clinical course, with a mortality rate of more than 50%.3 In the United States, the estimated incidence of this disease is 1.7 cases per million people per year; according to a review of 116 cases of mucormycosis, 22% are pulmonary mucormycosis.4 There are numerous predisposing clinical factors, such as uncontrolled diabetes mellitus, diabetic ketoacidosis, chemotherapy, haematological malignancies (leukaemia and lymphoma), immunosuppressive therapy, acquired or congenital neutropenia, antibiotic therapy, metabolic acidosis due to chronic salicylate intoxication, elastoplasty dressings, renal failure, prolonged postoperative period, solid tumours, solid organ transplantation, agammaglobulinaemia and burns.5-8 In patients with haematological malignancies, mucormycosis most commonly affects the lungs (58-81%).8
The diagnosis of pulmonary mucormycosis represents a challenge, as late diagnosis can have serious consequences. Therefore, it is of utmost importance to consider this disease among the possible differential diagnoses, especially in immunocompromised individuals. This article presents the case of a patient diagnosed by culture with mucormycosis.
Case presentation
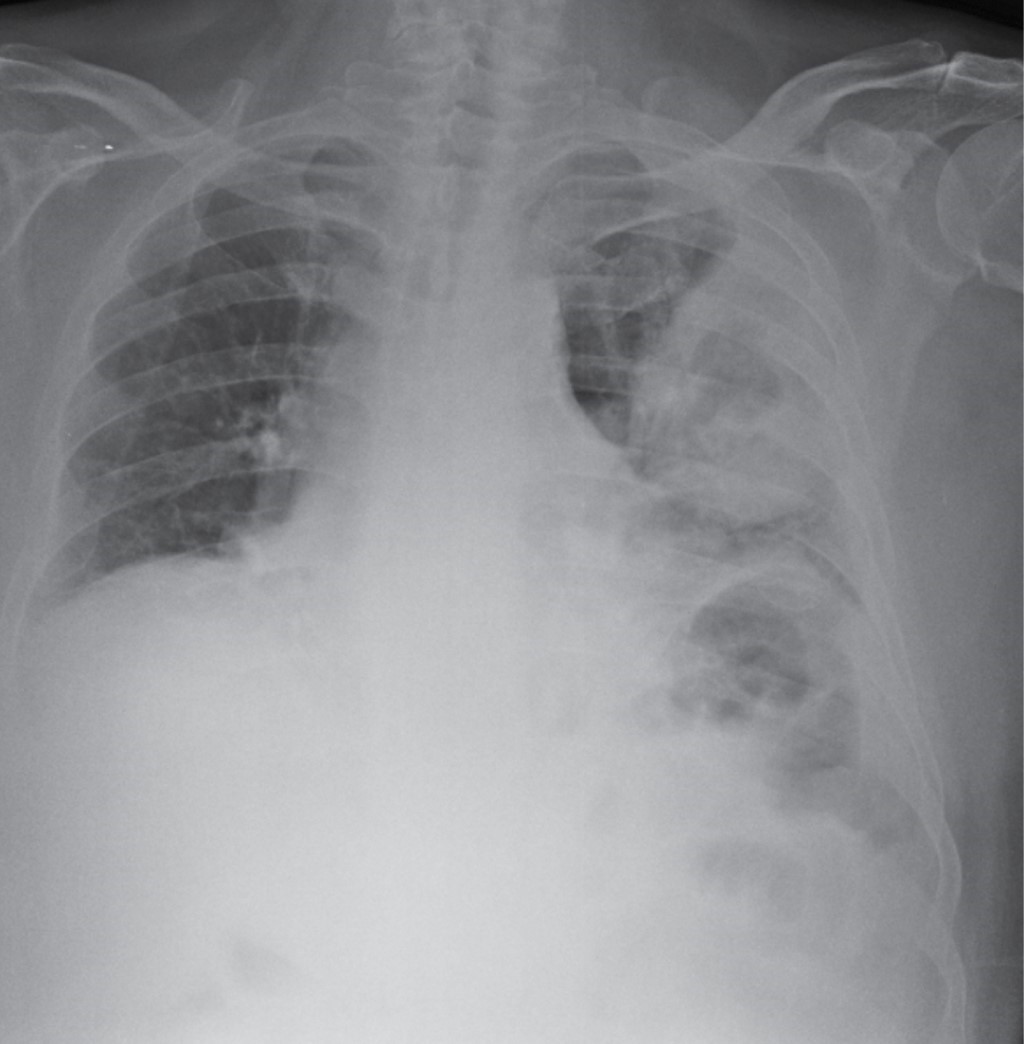
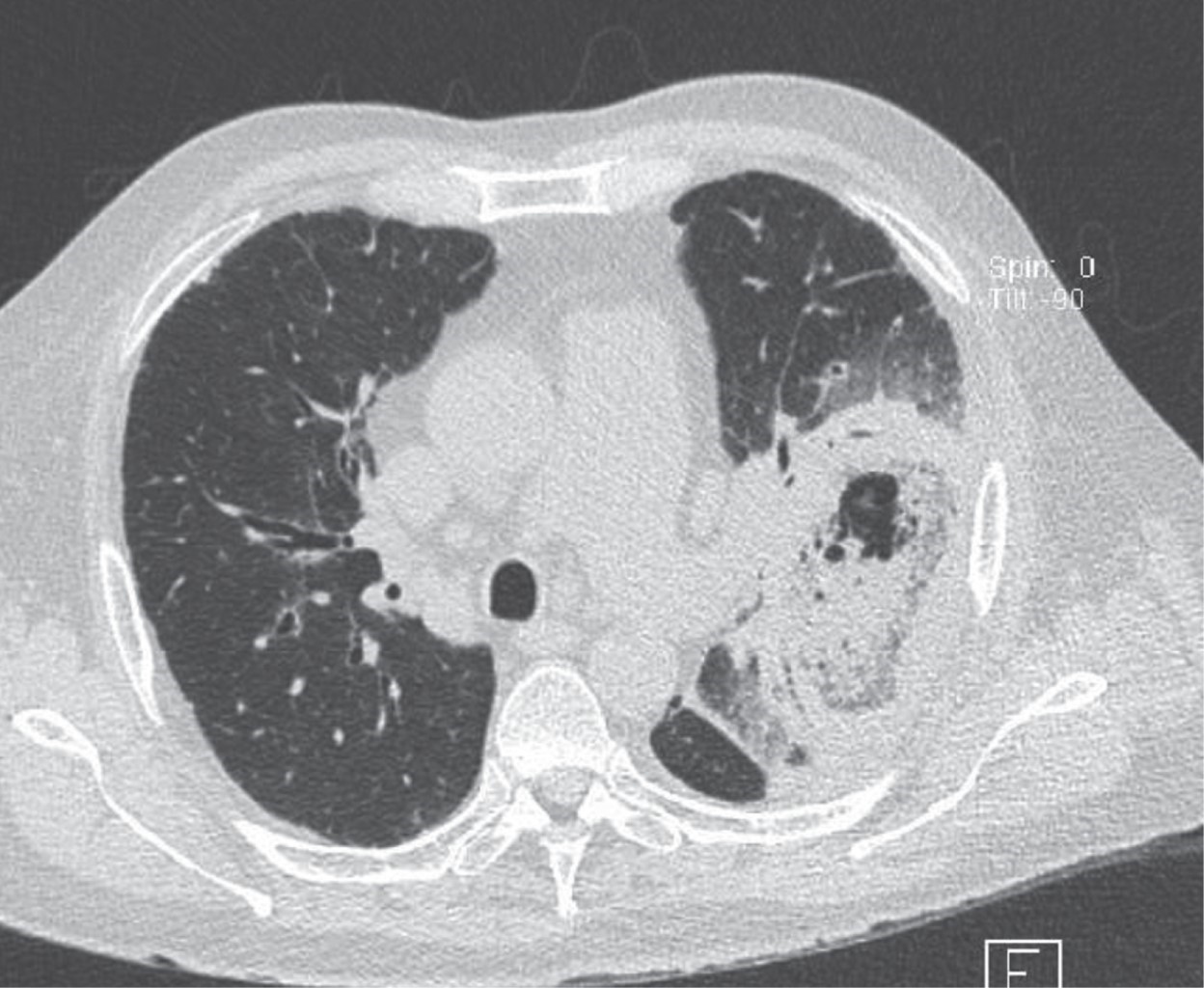
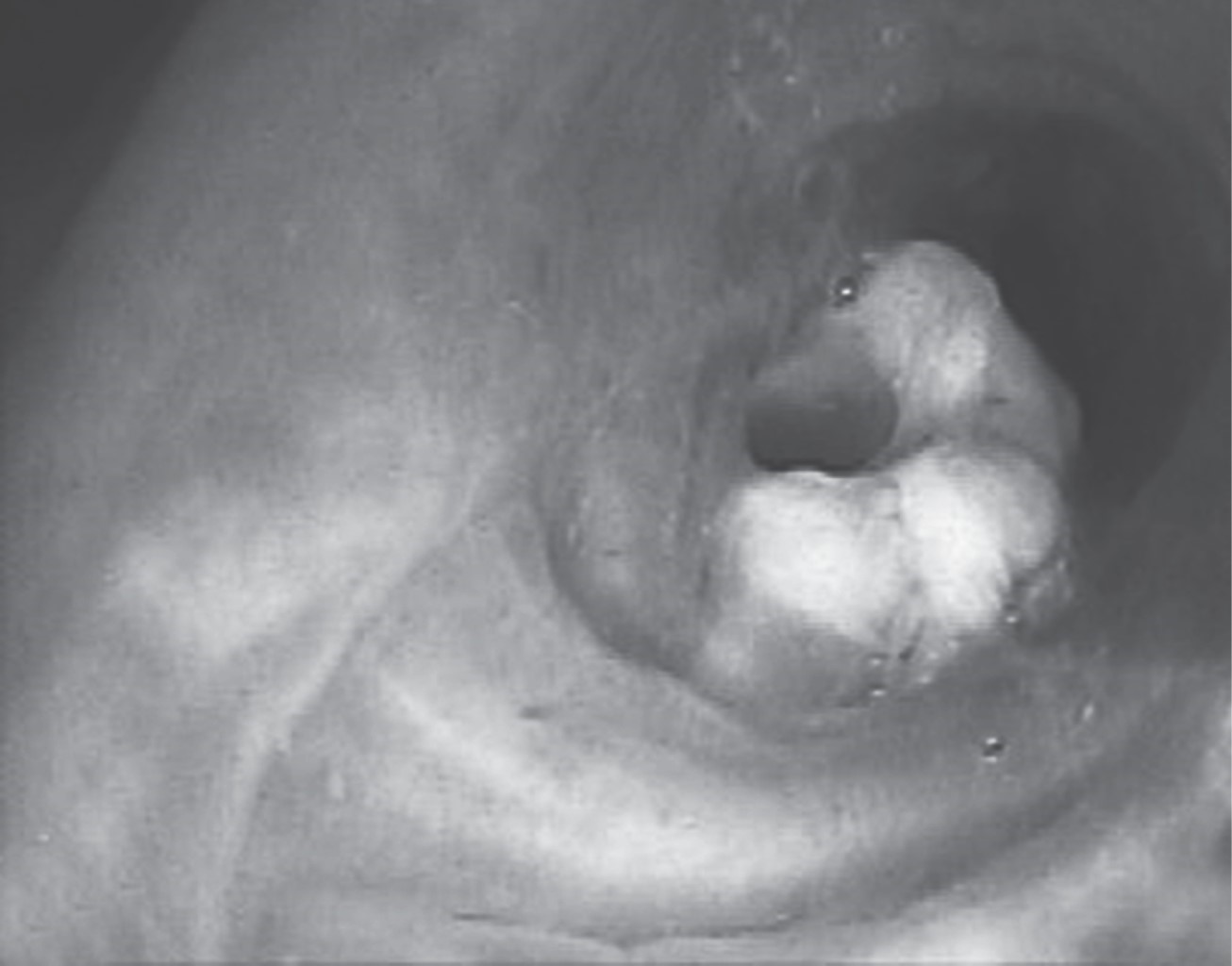
A 68-year-old man presented to our hospital in July 2023 with a non-productive cough with whitish expectoration, accompanied by dyspnoea on medium exertion; he denied fever and suffered a weight loss of 6 kg in the last few weeks. After receiving anti-infective treatment in the emergency department for two days, with little improvement, he was admitted to pneumology for diagnostic and therapeutic protocol; a chest X-ray was taken on admission (Figure 1); a chest CT scan was scheduled (Figure 2), where a well-defined cavitated mass was found within the left upper lobe, with the sign of the air like a crescent moon. Due to a suspected diagnosis of pulmonary tuberculosis, a bronchoscopy study was requested for bronchoalveolar lavage and acid-fast bacilli (AFB) test, mycobacterial and fungal cultures, as well as bacterial cultures. During the fibrobronchoscopy study, a whitish exophytic mass was observed in the anterior wall of the left S3 segment, so it was decided to take a biopsy and samples (Figure 3); subsequently, by histopathological study, the diagnosis of mucormycosis was made and, by culture, Absidia mucormycosis. Management with amphotericin B was started; during the first three days of treatment, the patient's oxygen requirement increased, a new chest X-ray was requested; he arrived at the 15-litre reservoir mask with 90% saturation, tachypnoea, respiratory rate 30 per minute, with thoracoabdominal dissociation, and advanced airway management was decided. He died of septic shock in the first 12 hours of his stay in respiratory intensive care.
Discussion
We present the case of a 68-year-old male patient with a history of type 2 diabetes mellitus with poor control as the only risk factor. Initially, a possible Mycobacterium tuberculosis infection was considered, so it was decided to perform a bronchoscopy to obtain bronchoalveolar lavage samples, while awaiting the results of acid-fast bacillus (AFB) and GenXpert tests. The pulmonary infiltration progressed and, due to positive mycology culture results for mucor, treatment with antifungal agents, including continuous amphotericin B, was initiated. Unfortunately, the patient received a late diagnosis of pulmonary mucormycosis and his prognosis proved fatal during intensive respiratory therapy.
Pulmonary mucormycosis develops due to inhalation of fungal spores in the bronchioles and alveoli, usually leading to rapid progression to pneumonia or endobronchial disease. In rare cases, this infection can lead to endobronchial lesions and complications associated with airway obstruction. Haemoptysis is a common symptom when vascular invasion occurs, which can sometimes be fatal. Symptoms of pulmonary mucormycosis are usually non-specific, even in advanced stages of infection, and may include fever, dyspnoea, cough and chest pain. Rarely, the disease may manifest as progressive subcutaneous emphysema, Pancoast syndrome, Horner syndrome or chronic mediastinitis and bronchial perforation.6,9
Patient immunosuppression appears to be the most critical risk factor predisposing the patient to mucormycosis. Diabetes is also considered an important risk factor, as it significantly decreases the function of the immune system and increases the risk of various infections.10
Pulmonary mucormycosis can cause pulmonary embolism because mucorales species tend to invade the elastic intima of large and small blood vessels, which can lead to thrombosis, bleeding and infarction. This may be an important diagnostic clue when pulmonary embolism of unknown cause occurs in patients with signs of pulmonary infection. Therefore, physicians should be alert and consider the possibility of pulmonary mucormycosis in these cases.
Radiological manifestations of pulmonary mucormycosis are mostly non-specific; more than 80% of patients show abnormal findings on chest radiographs.11 Findings may include consolidation, cavitation, air crescent sign, halo sign, inverted halo sign, multiple or solitary pulmonary nodules or masses, bronchopleural fistulas, pulmonary artery pseudoaneurysms, lymphadenopathy and pleural effusion. Cavitation is seen in up to 40% of cases, although the air crescent sign is rare. High-resolution computed tomography (CT) may be more sensitive in detecting the disease and may find evidence of infection earlier than conventional chest X-rays. The right lung is affected more frequently than the left, and there is a predilection for upper lobe involvement, although the reason behind this is unknown. The present case reported a right upper lobe lesion, as do the majority of cases in the literature.11
Histopathologically, vascular invasion with tissue necrosis and neutrophilic tissue infiltration is common to all types of mucormycosis. Diagnosis is made by demonstrating the presence of broad (6-16 µm diameter), non-septate (coenocytic), ribbon-like, right-angled branching hyphae in a routine haematoxylin and eosin stained tissue specimen. Special fungal stains are usually not necessary to establish the diagnosis. Less common and less specific features of pulmonary mucormycosis include bronchial invasion, pneumonia, lung abscesses and granulomatous pneumonitis.7
Conclusions
Pulmonary mucormycosis is primarily an opportunistic infection caused by mucorales. Such fungal infection occurs mainly in patients with immune system deficiency, although it may rarely attack immunocompetent patients. Due to its high mortality rate, clinicians must make judgements about suspected cases correctly and promptly to avoid misdiagnosis and delays in treatment. Early diagnosis of pulmonary mucormycosis remains a clinical challenge due to the lack of specific clinical manifestations. Firstly, clinicians need to be aware that pulmonary mucormycosis can occur in patients with normal immune function, especially when routine anti-infective treatments fail.
AFILIACIONES
1Hospital General de México. Mexico City, Mexico.Conflict of interests: the authors declare that they have no conflict of interests.
REFERENCES