Tracheobronchopathia osteochondroplastica as a cause of severe airway stenosis. Case report and literature review
Siado-Guerrero, Sergio Andrés1; Motta-Aguirre, María Paula2; Valverde-Cortés, Julián Andrés2; Lara-Sánchez, Rodrigo Armando2
Siado-Guerrero, Sergio Andrés1; Motta-Aguirre, María Paula2; Valverde-Cortés, Julián Andrés2; Lara-Sánchez, Rodrigo Armando2
ABSTRACT
Tracheobronchopathia osteochondroplastica is a rare condition, with an incidence rate between 0.25 and 0.3% in autopsy studies and approximately 0.01 to 0.8% in bronchoscopic findings. In our setting, we do not have specific statistics due to its rare presentation and diagnosis. Its etiology is still not well established, although it has been associated with immunoglobulin A deficiency and bone morphogenetic protein 2, as well as possible infections by bacteria or mycobacteria. Clinically, it is characterized by the appearance of osteocartilaginous nodular lesions in the submucosa of the central airways, which may protrude into the tracheal or bronchial lumen, generally causing nonspecific symptoms such as cough, hemoptysis, dyspnea, wheezing, and recurrent respiratory infections, and, as in the case of our patient, ventilatory failure. We present the case report of a patient who was admitted to our institution with a history of cough and dyspnea, leading to ventilatory failure, initially requiring non-invasive mechanical ventilation (NIMV). Further studies revealed the presence of calcified lesions and nodules in the upper airway on chest tomography. These lesions were confirmed by bronchoscopy, showing osteocartilaginous characteristics. The pathological report of the biopsy of these lesions was consistent with tracheobronchopathia osteochondroplastica. The patient was treated with antibiotic coverage and pneumatic dilations of the obstructive lesions in the upper airway. Subsequently, the patient showed adequate clinical improvement, resolving the ventilatory failure and being discharged without the need for supplemental oxygen or additional support.KEYWORDS
tracheobronchopathia osteochondroplastica, airway obstruction, tracheal stenosis, benign tracheal dysplasia.Abbreviations:
Introduction
Tracheobronchopathy osteochondroplastica (TO) is a rare disease characterized by the presence of osteocartilaginous nodules in the submucosa of the trachea and main bronchi.1-3 Despite its low incidence, estimated between 0.25 and 0.3% in autopsy studies,1,4-6 with a higher prevalence between the fourth and seventh decade of life.1,5,6 The initial symptoms are nonspecific and can be confused with asthma and sometimes with severe symptoms that can severely compromise respiratory function. The etiology of TO remains uncertain, although an association with immunoglobulin A deficiency and bone morphogenetic protein 2 has been suggested,6 its diagnosis is often challenging due to the nonspecific presentation of symptoms.5,7,8
Patients with TO may present with a variety of respiratory symptoms, including cough, hemoptysis, dyspnea and wheezing, which are often attributed to other more common diseases.3,5 In severe cases, TO can lead to airway obstruction and ventilatory failure,1 requiring medical and surgical intervention for its management.
In this report, we present a case of a patient with a diagnosis of TO, who was admitted to our institution with a clinical picture of persistent cough and progressive dyspnea that evolved to ventilatory failure. Through imaging studies and bronchoscopy, pathological features compatible with TO were identified and managed with pneumatic dilatation of the stenotic areas in order to prevent unnecessary resections with high risk of fistulas and progression of stenosis. This case highlights the importance of early diagnosis and proper management of this rare disease to prevent severe complications and improve patient outcomes.
Case presentation
A 76-year-old male patient was admitted to our institution with a clinical picture of one month of evolution, which was exacerbated in the last 15 days. Symptoms included cough with hemoptotic and mucopurulent expectoration, respiratory distress and progressive desaturation, with marked respiratory effort evidenced by the use of accessory muscles.
On admission to the Emergency Department, diagnostic studies revealed hypercapnic respiratory acidosis with partial metabolic compensation and hypoxemia: pH 7.293 (normal 7.35-7.45), PCO2 75.1 mmHg (35-45 mmHg), PO2 51.1 mmHg, HCO3-act 35.5 mmol/L (21-25 mmol/L), SO2 83.6%, and PaO2/FiO2 ratio of 1.60 mg/dL. The CBC showed no evidence of leukocytosis or neutrophilia, with a leukocyte count of 7.14 × 103/µL (normal 3.7-10.1), %neutrophils 69.0% (39.6-73.3%), %lymphocytes 21.8% (18.0-48.3%), hemoglobin 13.0 g/dL, hematocrit 44.3%, and platelet count 472 × 103/µL.
Chest CT (Figure 1) showed bilateral parahilar interstitial reticular interstitial opacities, more accentuated in the left lung field, extending towards segments V, VIII, IX and X, with occupation of the alveolar space, increased density of the lung parenchyma and presence of air bronchogram. In addition, a calcified lesion dependent on the lateral wall was identified at the level of tracheal ring 8, of approximately 2 cm, which protrudes into the tracheal lumen.
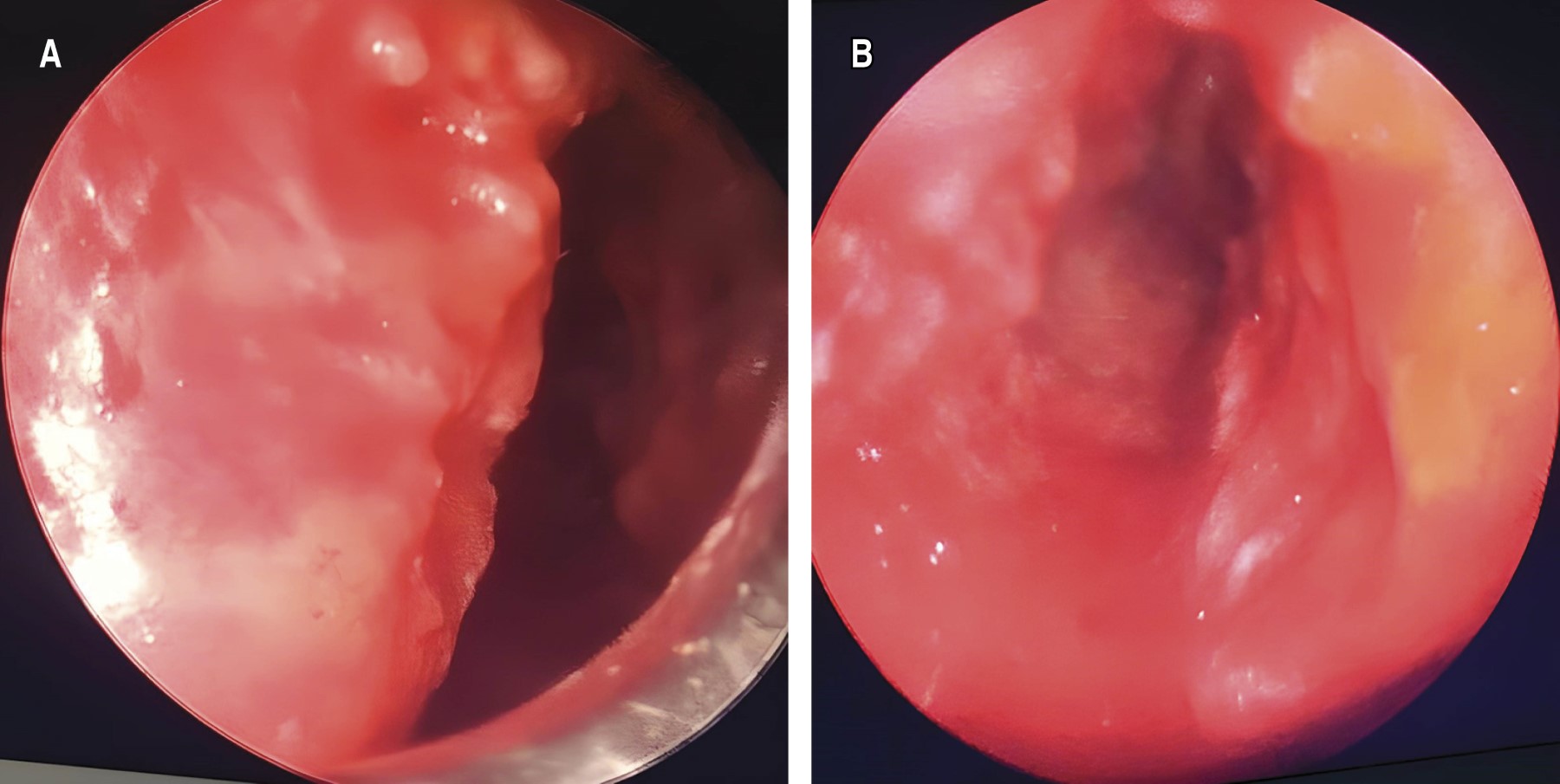
Given the above, ventilatory failure was considered secondary to left basal pneumonia, exacerbated by tracheal stenosis, which required management with noninvasive mechanical ventilation (NIMV). He was evaluated by the Pneumology Service, which recommended fibrobronchoscopy for microbiological study and sampling. The fibrobronchoscopy showed a mucosa with a fibrotic lesion dependent on the lateral wall, of hard consistency, located 2 cm from the vocal cords, which compromised 80% of the tracheal lumen. In addition, distal to the lesion, an infiltrated and indurated mucosa was evidenced, with multiple whitish nodular lesions protruding into the tracheal lumen, respecting the posterior wall of the trachea and hindering the passage of the bronchoscope.
The biopsies taken showed a tracheal wall lined by respiratory epithelium without dysplasia, arranged in a lax stroma, with mature hyaline cartilage without histopathological alterations. No granulomas or neoplastic cells were observed. Bronchoalveolar lavage culture was negative for fungi and polymerase chain reaction (PCR) molecular test for Mycobacterium tuberculosis was not detected.
The patient was evaluated by the Thoracic Surgery Service, which decided to perform an endoscopic resection of the tracheal lesion. During the procedure, tracheal stenosis was evidenced 2 cm from the trachea, with a lesion dependent on the left lateral and anterior wall of the trachea (Figure 2), of hard and calcified consistency, in addition to multiple cobblestone-like lesions. The procedure was performed without complications.
Subsequently, the patient continued with an adequate clinical evolution, receiving antimicrobial management due to suspicion of pneumonic process and without requiring new cycles of NIMV. There was an improvement in blood gases, with correction of respiratory acidosis (pH 7.377) and a decrease in pCO2 to 67.7 mmHg, with a PaO2/FiO2 ratio of 288 mmHg. He was discharged and evaluated in outpatient follow-up one month after the procedure, without respiratory distress or inspiratory stridor, and with an adequate respiratory pattern.
Discussion
TO is a rare airway pathology, characterized by benign dysplasia of the trachea and main bronchi, first described by Rokitansky7 in 1855 and, later, in 1957 described microscopically by Wilks.5,9,10 In 1910 Achoff called it "osteoplastic tracheopathy"10 and, later, in 1964 Secrest and coworkers gave it the current name TO.2 To date, its etiology has not been clarified, but hypotheses have been generated suggesting that it is associated with autoimmune pathologies such as thymoma, chronic atrophic rhinitis, amyloidosis, lymphomas, epidermal cysts and myasthenia gravis.6,7 In our patient's case, no autoimmune pathologies were identified at the time of diagnosis; however, he did present pulmonary infectious symptoms as described in the literature, which is characteristic of this pathology, exacerbations due to recurrent pulmonary infections.
Radiologically it is characterized by cartilaginous calcification of the walls of the main airways that protrudes into the lumen in a "stone garden" appearance,6 except for the posterior membranous wall,6 which were the findings evidenced in the CT scan of the patient we present in this case; in addition, its age of presentation is found in patients between 40 and 80 years of age.5,6 Our patient is in this age range given that he is 76 years old and the bronchoscopic findings showed whitish nodular lesions that protruded into the tracheal lumen, respecting the posterior wall of the trachea; in addition, the surgical procedure showed the classic description of cobblestone mucosa, which is consistent with what is described in the literature.
Clinical symptoms are usually nonspecific, ranging from asymptomatic, presenting with chronic cough, hemoptysis, to severe symptoms such as airway obstruction leading to ventilatory failure;7 our patient presented with cough, hemoptysis and dyspnea, leading to ventilatory failure, probably exacerbated by a concomitant pneumonic process that generated a decrease in the stenosis caliber due to accumulation of secretions, which worsened his symptoms.
The literature establishes tracheobronchial amyloidosis as the main differential diagnosis, and others such as papillomatosis, endobronchial sarcoidosis, Wegener's disease, which, like amyloidosis, do not respect the posterior wall of the trachea, unlike TO, which does respect the posterior wall of the trachea..3,6,7,11,12 In our patient the tomographic and endoscopic findings are consistent with the posterior wall being completely respected, which further supports the diagnosis of TO; in addition, other possible differential diagnoses such as calcified tuberculous granulomas ruled out by PCR for negative Mycobacterium and histopathology without evidence of granulomas were ruled out. The literature describes in the histopathological findings, the presence of calcium phosphate in the submucosa and benign proliferations of bone and cartilage, squamous metaplasia can also be identified.10 In the case of the patient in this report, histopathology identified the presence of tracheal wall lined by respiratory epithelium without dysplasia, arranged in a lax stroma, with mature hyaline cartilage without histopathological alterations in accordance with what has been reported in the literature.2
Treatment depends on the symptoms presented by the patient and the response to each of the previously performed, requiring inhaled corticosteroid therapy, recurrent antibiotic management,6 endobronchial laser resection, tracheal stent placement,12 tracheal resection or tracheostomy; however, there is no definitive treatment to cure this pathology.6,7 Our patient initially required bronchodilator therapy and corticosteroid associated with NIMV; and given the endoscopic findings of 80% obstruction of the tracheal lumen associated with signs of ventilatory failure, it was decided to perform endotracheal laser resection with adequate clinical response, resolving the imminence of ventilatory failure, with improvement in blood gases and without requiring the use of NIMV. One month after the procedure, the patient was evaluated on an outpatient basis, finding no symptoms of respiratory distress.
Conclusions
TO is a rare disease of infrequent presentation and non-specific respiratory symptoms that can have a significant impact on the quality of life of patients due to the airway obstruction it produces. Diagnostic studies, including chest tomography and bronchoscopy, are necessary to exclude other differential diagnoses, up to histopathological study. Although its etiology remains unknown and there is no definitive treatment, a multidisciplinary approach and appropriate management can lead to a significant improvement in the quality of life of patients. Continuous surveillance and periodic evaluation are essential to effectively manage this rare and complex condition.
AFILIACIONES
1Medilaser Clinic, Neiva, Huila. Thoracic Surgery Fellow, Universidad El Bosque. Bogota, Colombia 2Medilaser Clinic, Neiva, Huila, Colombia.Acknowledgments: to Clínica Medilaser de Neiva, Dr. Milton Jiménez.
Conflict of interests: the authors declare that they have no conflict of interests.
REFERENCES
García CA, Sangiovanni S, Zúñiga-Restrepo V, Morales EI, Sua LF, Fernández-Trujillo L. Tracheobronchopathia osteochondroplastica-clinical, radiological, and endoscopic correlation: case series and literature review. J Investig Med High Impact Case Rep. 2020;8:2324709620921609. doi: 10.1177/2324709620921609.